The Revenue Cycle Blog
Filter By
- ABA Therapy Billing
- AI in Medical Billing
- AI in Revenue Cycle
- Accounts Receivable Management
- Accounts Receivable Mangement
- Allergy and Immunology Billing Services
- Anesthesia Billing Services
- Back Office Revenue Cycle
- Bariatric Surgery Billing
- Billing For Physician Practice and Medical Groups
- Billing for Physician Practices and Medical Groups
- Blog
- COVID-19 Billing
- CPT Codes
- Cardiology Billing Services
- Charge Capture Services
- Charge Entry - Medical Billing
- Charge Entry Services
- Clinical Documentation Improvement - CDI
- Clinical Documentation Integrity
- Company News
- Credit Balance Services
- DME Billing Services
- Denial Code CO-97
- Denial Management - Medical Billing
- Dermatology Billing Services
- E&M
- Electronic Health Records
- Eligibility and Benefits Verification Services
- Emergency Department Billing Services
- FAQs
- Family Practice Billing Services
- G Code
- Gastroenterology Billing Services
- General Surgery Billing Services
- HCC Coding
- HCC Coding Services
- HCPCS
- Healthcare Collections
- Hospitals
- Internal Medicine Billing Services
- Medical Billing Company
- Medical Billing Services
- Medical Billing Services in California
- Medical Billing Services in Texas
- Medical Claim Submission
- Medical Coding Services
- Mental Health Billing Services
- Mental health Billing Services
- Mid Cycle in Revenue Cycle
Hepatocellular Carcinoma HCC in Medical Coding: Complete ICD-10 Guide
Hepatocellular Carcinoma HCC in medical coding involves assigning ICD-10 code C22.0 for primary liver cancer diagnosis. This guide explains ICD-10 codes, documentation, sequencing, billing, and reporting requirements for proper oncology coding and reimbursement.
Optometry Billing and Coding Cheat Sheet for Hospital (2026)
Hospital optometry billing in 2026 requires proper coding, accurate documentation, and compliance with medical billing rules. This Optometry Billing and Coding Cheat Sheet covers E/M codes, ICD-10, modifiers, and billing guidelines to help reduce denials and improve reimbursement in hospital settings.
Gastroenterology Billing: Screening vs Diagnostic Colonoscopies
Gastroenterology Billing for screening and diagnostic procedures requires correct classification and coding. Screening applies preventive care, while diagnostic applies symptom-based necessity, and therefore billing and reimbursement differ. Proper billing helps reduce denials and improves claim approval.
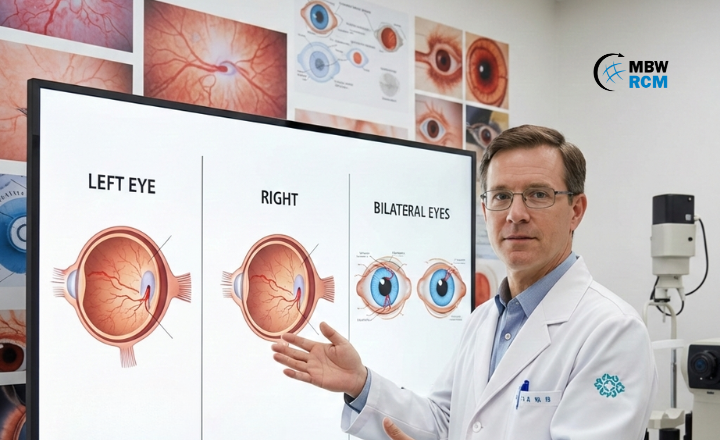
Retinal Detachment ICD 10 Code for Left, Right & Bilateral Eyes
Retinal Detachment ICD 10 Code for Left, Right & Bilateral Eyes explains diagnosis code selection based on detachment type, laterality, and clinical documentation. This blog covers commonly used ICD-10 codes, eye-specific coding differences, and key documentation points for retinal detachment diagnosis and ophthalmology billing.
How to Choose the Best RCM Vendor USA for Healthcare Providers
Looking for a scalable RCM vendor USA to support your growing healthcare organization? MBW RCM strengthens end-to-end revenue cycle performance.
Top 20 CPT Codes for Gastroenterology Clinics (2026 Guide)
Stay ahead in 2026 with the Top 20 CPT Codes every gastroenterology clinic should know. Learn which high-volume GI procedures drive revenue, reduce denials, and support stronger documentation and billing performance.
Practice Care Podcast: Vinny Sankaran on AI Voice in RCM
Vinny Sankaran joins the PracticeCare podcast to discuss how AI voice, automation, and emerging technologies are reshaping revenue cycle management and helping healthcare organizations improve performance and scalability.
Ocular Trauma ICD-10: Do’s & Don’ts in Medical Coding
Ocular trauma ICD-10 coding requires careful attention to injury type, laterality, and treatment phase. This blog covers essential Do’s and Don’ts to help reduce coding errors and support correct eye injury code selection in real-world scenarios.
How Gastroenterology RCM Reduced A/R by 42 Days: Explained Step-by-Step
Gastroenterology practices often struggle with high A/R due to payer rules, authorization delays, and coding complexity. This blog explains how targeted revenue cycle improvements helped reduce A/R by 42 days by strengthening eligibility verification, coding accuracy, and denial prevention across GI billing workflows.
Top 10 Gastroenterology Billing Company in USA
Gastroenterology billing requires specialized coding accuracy, payer expertise, and strong denial management to maintain consistent reimbursements. Choosing the right gastroenterology billing company can directly impact financial performance and billing efficiency. This blog highlights top companies supporting GI practices with accurate workflows, reduced denials, and improved revenue cycle outcomes.
Top 5 Ophthalmology Medical Billing Challenges in Healthcare
Ophthalmology Medical Billing requires accurate coding, strong documentation, and payer compliance. Challenges like Eye vs E/M coding, diagnostic bundling, drug reimbursement risks, and authorization errors can impact revenue. Understanding these billing challenges helps practices reduce denials, improve claim accuracy, and maintain consistent reimbursement.
Top 10 Ophthalmology Billing Companies in USA
Explore the top ophthalmology billing companies in the USA and how specialty-focused billing partners help reduce denials, improve coding accuracy, and strengthen revenue performance for cataract, retina, and glaucoma services.
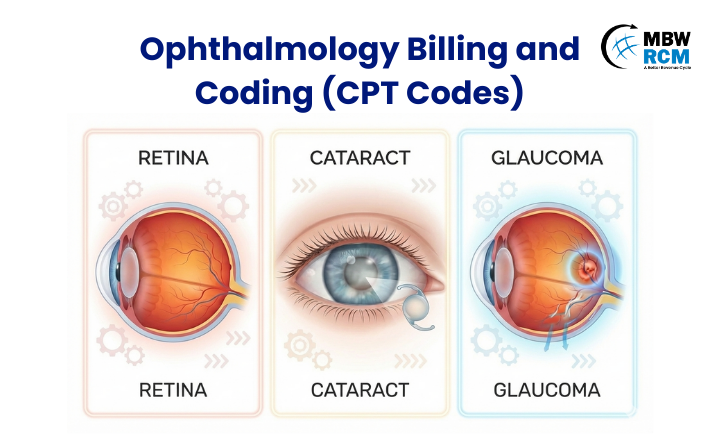
Ophthalmology Billing and Coding for Retina, Cataract and Glaucoma Services
Ophthalmology billing and coding for retina, cataract, and glaucoma services demand careful CPT selection, modifier use, and documentation. This guide outlines key requirements and best practices to help practices reduce denials and maintain consistent reimbursement.
What Is a Specialty Code in Medical Billing?
A specialty code in medical billing identifies a provider’s area of practice and plays a key role in claims processing, reimbursement, and compliance. This guide explains specialty codes, how they differ from taxonomy codes, common types, and how errors lead to denials and revenue loss.
Why Practices Outsource Family Practice Billing Services to MBW RCM
OB/GYN billing services for hospitals help reduce maternity billing errors, prevent denials, and improve reimbursement accuracy across extended episodes of care.
OB/GYN Billing Services for Hospitals: Fixing Denials Across Episodes of Care
OB/GYN billing services for hospitals help reduce maternity billing errors, prevent denials, and improve reimbursement accuracy across extended episodes of care.
Top 10 OB/GYN Revenue Cycle Management Challenges in Healthcare
Explore the biggest OB/GYN revenue cycle management challenges impacting health systems, from maternity billing and denials to authorization and patient collections.
Top 5 Cost to Collect Revenue Cycle Benchmark Standards in Medical Billing
Cost to collect benchmarks play a key role in evaluating billing efficiency across healthcare organizations. This blog outlines the top cost to collect revenue cycle benchmarks for billing, with practical ranges by practice size, specialty, payer mix, and billing model to support informed revenue cycle decisions.
Top 10 OBGYN Medical Billing Company in US
Managing OB-GYN billing requires specialty expertise. Explore the top 10 OBGYN medical billing Company options in 2026 and discover why MBW RCM is the leading choice for women’s health practices.
What Is Revenue Cycle Management (RCM) in Healthcare Billing?
Revenue cycle management is central to healthcare billing and reimbursement. This article explains what it is, why it matters, and how key stages—from patient access to payment follow-up—work together, along with common challenges, metrics, and the role of technology in billing operations.