All-in-One Charge Entry in RCM Guide for 2025
Charge Entry in RCM is the process of recording healthcare services into a billing system to prepare claims for insurance. To put it another way, it's like turning patient visits into digital invoices. If done properly, it helps clinics get paid faster. If errors occur, then claims can be rejected or delayed. Accordingly, learning charge entry is the first thing every billing professional should understand in 2025.
Table of Contents
What Is Charge Entry in Rcm With an Example?
Charge Entry in RCM (Revenue Cycle Management) is the process of entering all services, procedures, and treatments a patient receives into the healthcare provider’s billing software. This step happens after medical coding and before claim submission, forming a critical bridge between clinical care and reimbursement.
Each entry in this phase includes essential information such as:
Patient demographics
Insurance details
Diagnosis codes (ICD)
Procedure codes (CPT/HCPCS)
Date and place of service
Rendering provider information
The goal is to properly record each billable service with the correct codes so insurance companies clearly understand the charges, helping reduce denials, delays, or payment issues.
Example of Charge Entry in RCM:
Scenario: A patient visits an orthopedic clinic complaining of knee pain after a sports injury.
The provider performs an evaluation and prescribes an X-ray.
The medical coder reviews the provider’s documentation and assigns:
ICD-10 Code: M25.561 (Pain in right knee)
CPT Code: 99213 (Office or other outpatient visit)
CPT Code: 73562 (X-ray of knee, 3 or more views)
The charge entry specialist or billing team enters this data into the billing system — along with the patient's name, visit date, insurance provider, and rendering physician.
The software validates the entries, and the data is passed along to the claims team for submission to the insurance company.
Importance of Charge Entry in Medical Billing
Charge entry is important in medical billing—it turns coded services into billable claims. If skipped or done incorrectly, it can cause denials, delays, or payment issues. It connects coding to claim submission, helping ensure insurance companies understand the charges so providers get paid faster and more smoothly. If you’re unsure how charge entry impacts your billing cycle, read here Why Charge Entry in Medical Billing Matters to understand its role and impact.
When does charge entry occur in medical billing?
Charge Entry in RCM happens after the provider documents the visit but before the claim is submitted to insurance. It is the stage where all coded information is converted into billable charges in the system. To clarify, this means charge entry occurs between medical coding and claim submission in the billing cycle.
After the Patient Visit
Once the patient’s appointment ends, the provider completes their documentation — including diagnosis, procedures performed, and any medical decisions made. These details are then reviewed by coders, who assign appropriate CPT (Current Procedural Terminology) and ICD (International Classification of Diseases) codes.
At this point, the information becomes ready for charge entry, which involves inputting the codes and service data into the billing system.
Example: A doctor sees a patient for a sprained ankle. The coder assigns ICD code S93.4 (sprain of ankle), and CPT code 99213 (office visit). These are then entered during charge entry.
Before Claim Submission
Only after the charges are entered and validated can the claim be generated and sent to the payer. If the charge entry includes errors — such as missing codes, mismatched dates, or wrong patient data — the billing process will be delayed or stopped.
For this reason, charge entry is considered a checkpoint step: everything must be reviewed and completed here before a claim goes out.
Charge Entry Timing in the Medical Billing Process
| Stage | What Happens at This Stage | Position in the Workflow |
|---|---|---|
| Patient Visit | The provider examines the patient and offers treatment | First step |
| Provider Documentation | The provider records what was done — notes, diagnosis, procedures | After visit, before coding |
| Medical Coding | Coded entries (CPT/ICD) are assigned based on provider notes | After documentation, before charge entry |
| Charge Entry | All services and codes are entered into billing software | After coding, before claims submission |
| Claim Submission | The completed charges are sent to the insurance company | After charge entry |
Who Is Responsible for Charge Entry in RCM?
Charge Entry in RCM is usually completed by specialized administrative staff who are trained to handle patient information, procedure codes, and billing software. Depending on the size and setup of a healthcare organization, this task may fall to different people.
In Small Clinics or Independent Practices
In smaller clinics, charge entry is often performed by medical billers, office managers, or cross-trained administrative staff. These individuals usually wear multiple hats — handling patient check-ins, insurance verification, and charge input.
Since small teams manage many tasks, charge entry might be entered manually into billing software shortly after each patient visit.
Example: In a 3-provider family clinic, the front desk manager may complete charge entry at the end of the day after reviewing provider notes and codes.
If you are interested to read more about charge entry, please have a look at this case study on ‘‘Improved Revenue Cycle Workflow Accelerates Reimbursements’’.
In Larger Medical Facilities or Hospitals
In bigger organizations like hospitals, urgent care chains, or multi-specialty groups, charge entry is assigned to dedicated billing departments. These departments may include:
Medical billers
Charge entry specialists
Remote billing teams or BPOs (outsourced vendors)
In such settings, charge entry happens within 24–48 hours of the patient visit and goes through a quality check process before the claim is filed.
Fun Fact: Some large billing teams handle thousands of charge entries per day using electronic health records (EHRs) integrated with billing software.
Can Charge Entry Be Outsourced?
Yes. Many providers choose to outsource charge entry to third-party medical billing companies. These companies use secure portals to receive documentation, assign codes, and enter charges — often with faster turnaround and reduced in-house workload.
“Charge entry: where numbers and healthcare collide — no stethoscope required.”
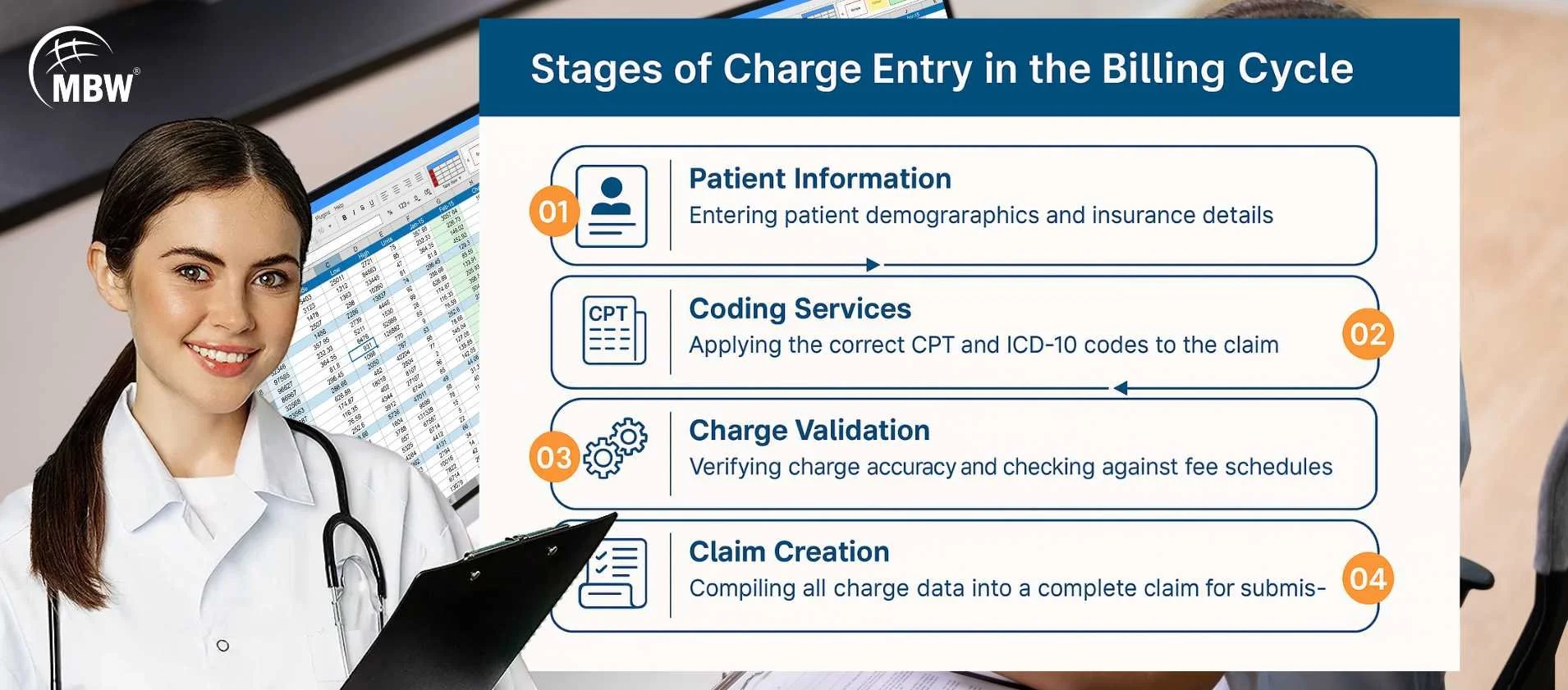
Step-by-Step Charge Entry Process (2025 Update)
To correctly submit claims and avoid billing issues, it's important to understand how charge entry in RCM works. Below is a simple breakdown of each step in the charge entry process to help prevent common errors and delays.
Collect Documentation
Before anything can be entered, you need the provider's documentation. This includes patient notes, procedures performed, diagnoses, and any treatments given during the visit. This information is crucial because it links each charge directly to what happened during the appointment and supports overall billing quality. Common issues such as missing or incorrect diagnostic details at this stage can lead to downstream errors, making it important to address diagnostic test errors in charge entry early in the process.
Apply CPT and ICD Codes
Next, medical coders assign the proper CPT (procedure) and ICD (diagnosis) codes. These codes represent what the provider did and why it was done. They must be accurate so that the insurance company understands the services being billed.
Enter Charges into Software
Once the codes are assigned, the charges are entered into billing software. This step prepares the data for claim creation. The patient’s name, date of service, provider name, and all codes are added to the digital claim.
Review Data for Mistakes
Before moving forward, everything entered must be double-checked. This includes verifying codes, checking for typos, and making sure no information is missing. Reviewing helps prevent claim rejections or denials from the insurance company.
Save and Send to Billing Team
After the review is complete, the charges are saved and sent to the billing or claims department. This team will generate and submit the insurance claim using the charge entry information. At this point, the claim moves to the next stage of the billing cycle.
Altogether, each step in the charge entry process must happen in the correct order. If anything is skipped or done out of sequence, then the billing team may face delays, rework, or even payment denials. For a more detailed explanation of workflows and best practices, explore the complete charge entry process in medical billing.
Tools and Software Used in Charge Entry
Popular billing platforms like Kareo, AdvancedMD, DrChrono, NextGen, and eClinicalWorks help manage charge entry by organizing patient data and service codes. These systems offer features like CPT code search, insurance checks, and error alerts, which speed up data entry and reduce mistakes.
Common Errors in Charge Entry (and Fixes)
Even small mistakes in charge entry in RCM can lead to claim rejections, delays, or payment issues. Identifying these errors early helps prevent billing complications later in the process. Below are some of the most common charge entry mistakes and how to correct them effectively.
| Error | What Happens | How to Fix It |
|---|---|---|
| Wrong CPT/ICD codes | Claim rejection | Use updated codebooks and cross-check |
| Missing insurance info | Denial or delay | Confirm insurance during check-in |
| Duplicate charge entries | Overbilling risks | Use software alerts and verify totals |
| Missing modifiers | Partial payment | Review procedures that need modifiers |
| Skipped authorization link | Full claim denial | Attach prior approvals before submission |
After that, a second review is helpful before finalizing the charges.
How Does Charge Entry Impact Medical Billing?
The quality of charge entry directly impacts whether claims are accepted, delayed, or adjusted by insurance companies. If this step is rushed or done incorrectly, the billing cycle can slow down or result in financial losses for the provider. Here's how poor charge entry can affect outcomes:
Rejections
If the wrong CPT or ICD codes are entered — or if information is missing — insurance companies will reject the claim outright. Rejected claims must be corrected and resubmitted, which delays payment and increases administrative workload.
Delayed Payments
When charge entry lacks critical details like service dates, modifiers, or patient insurance data, the claim may be held up for clarification. This delays the payment process and may push the claim past timely filing limits, risking non-payment altogether.
Claim Edits and Underpayments
Even if a claim is accepted, incorrect charge data can lead to lower reimbursement. For example, missing a modifier or entering the wrong unit count may result in the payer reducing the allowed amount. These edits can be hard to track and may go unnoticed without proper review.
“Forget dragons — the real monsters are mismatched CPT codes.”
Simple Tips to Improve Charge Entry in 2025
Always use the latest CPT and ICD codebooks
Verify insurance details before entering charges
Review each charge carefully before submission
Don’t copy and paste charge data without checking it
Train or refresh billing staff every 6 months
Following these tips regularly can help reduce rework and improve the overall accuracy of your billing process.
To conclude, understanding charge entry in RCM helps reduce claim rejections and payment delays. By entering each service correctly, checking for common errors, and using reliable tools, you can make the billing process more efficient. Whether you're just getting started or improving your current approach, applying these steps will help you handle charge entry more clearly and with better results.
If you're looking for charge entry services or end-to-end billing, MBW RCM offers dependable support and experienced teams to assist at every stage.
📞 Contact MBW RCM today to learn how we can support your workflow and keep your billing on track.
Frequently Asked Questions on Charge Entry in RCM
You need documentation from the provider, CPT/ICD codes, and patient insurance details.
Coding assigns the right codes; charge entry involves putting those codes and service info into the billing system.
Medical billers, coding assistants, or billing specialists usually handle it, depending on practice size.
Some tools assist with auto-fill features, but manual review is still needed.
It should be reviewed before every claim submission — daily or weekly based on practice volume.
Request for Information
Reduce billing errors and improve charge accuracy. Fill out the form to receive a custom quote or request a live demo of MBW RCM’s charge entry solutions.