The Revenue Cycle Blog
Filter By
- ABA Therapy Billing
- AI in Medical Billing
- AI in Revenue Cycle
- Accounts Receivable Management
- Accounts Receivable Mangement
- Allergy and Immunology Billing Services
- Anesthesia Billing Services
- Back Office Revenue Cycle
- Bariatric Surgery Billing
- Billing For Physician Practice and Medical Groups
- Billing for Physician Practices and Medical Groups
- Blog
- COVID-19 Billing
- CPT Codes
- Cardiology Billing Services
- Charge Capture Services
- Charge Entry - Medical Billing
- Charge Entry Services
- Clinical Documentation Improvement - CDI
- Clinical Documentation Integrity
- Company News
- Credit Balance Services
- DME Billing Services
- Denial Code CO-97
- Denial Management - Medical Billing
- Dermatology Billing Services
- E&M
- Electronic Health Records
- Eligibility and Benefits Verification Services
- Emergency Department Billing Services
- FAQs
- Family Practice Billing Services
- G Code
- Gastroenterology Billing Services
- General Surgery Billing Services
- HCC Coding
- HCC Coding Services
- HCPCS
- Healthcare Collections
- Hospitals
- Internal Medicine Billing Services
- Medical Billing Company
- Medical Billing Services
- Medical Billing Services in California
- Medical Billing Services in Texas
- Medical Claim Submission
- Medical Coding Services
- Mental Health Billing Services
- Mental health Billing Services
- Mid Cycle in Revenue Cycle
Verifying Insurance Eligibility for Detecting Plan Exclusions Before Treatment
Plan exclusions often cause denied claims when identified too late. Insurance benefits verification Services help identify coverage limits and non-covered services before treatment. Early exclusion detection reduces denials, rework, and billing issues. This blog explains how insurance benefits verification Services identify plan exclusions before treatment to reduce denials.
Top 8 strategies for patient insurance Benefits verification to reduce claim denials
Many claim denials start at the front desk. Incomplete patient insurance benefits verification leads to eligibility errors, missing authorizations, and unpaid claims. This blog shares eight practical strategies to strengthen verification, prevent denials, and improve clean claim rates.
Insurance Benefit Verification for Multi-Plan and Secondary Coverage Checks
Patients with multiple insurance plans often require added attention during coverage review. Insurance Benefit Verification helps determine primary and secondary payer responsibility, confirm eligibility, and review coordination of benefits. This blog explains how multi-plan and secondary coverage checks work, common challenges providers face, and practical approaches to support smoother billing and clearer insurance handling.
6 Validation Steps for Recurring Treatments in Eligibility Verification in Medical Billing
Recurring treatments require repeated eligibility checks to prevent coverage gaps, expired authorizations, and benefit exhaustion. This blog outlines six validation steps for recurring eligibility verification in medical billing to track coverage, visit limits, and patient responsibility while reducing claim denials.
Integrating Outsourced Insurance Eligibility Verification Services with Billing & EHR Systems
Integrating Outsourced Insurance Eligibility Verification Services with billing and EHR systems helps healthcare organizations manage eligibility data where daily work takes place. This article highlights how eligibility information flows between systems, common integration challenges, security considerations, and best practices that support consistent billing preparation and documentation.
Automated Insurance Eligibility Verification for Clinics Handling Same-Day Appointments
Same-day appointments leave little room for insurance errors. Clinics must verify coverage quickly while managing walk-ins and packed schedules. Automated insurance eligibility verification helps confirm coverage in real time, reduce intake delays, and prevent billing issues after the visit. This blog explains how eligibility automation supports same-day workflows and front desk efficiency.
How Surgical Teams Handle the Eligibility Verification Process in Medical Billing
Surgical teams follow a structured approach to confirm insurance coverage, review benefits, and meet payer requirements before procedures. Understanding the Eligibility Verification Process in Medical Billing helps reduce scheduling issues, prevent billing delays, and support clean surgical claims.
Patient Insurance Verification: What Happens When You Skip It?
Skipping patient insurance verification can lead to denied claims, delayed payments, and increased follow-up work weeks after a visit. This blog explains how missed verification affects billing, scheduling, and front desk workflows, and outlines the common challenges healthcare practices face when insurance details are not confirmed in advance.
How Insurance Verification Improves Patient Intake Efficiency for Multi-Location Clinics
Insurance verification helps improve patient intake efficiency for multi-location clinics by reducing intake delays and shortening check-in time. This blog explains how early verification, standardized processes, and automation support consistent patient flow across multiple clinic locations.
How Insurance Eligibility Verification Services Prevent Same-Day Claim Rejections
Same-day claim rejections often occur due to eligibility issues identified too late in the billing process. This blog explains how Insurance Eligibility Verification Services help prevent these rejections by validating insurance details before claims are created, reducing errors, rework, and delays in claim processing.
How To Verify Patient Insurance Eligibility Verification
Patient insurance eligibility verification involves reviewing coverage status, benefits, network participation, and payer requirements before services are provided. This blog explains key verification checks that support accurate scheduling decisions and billing preparation.
Insurance Eligibility Verification Checklist Every Front Desk Should Use
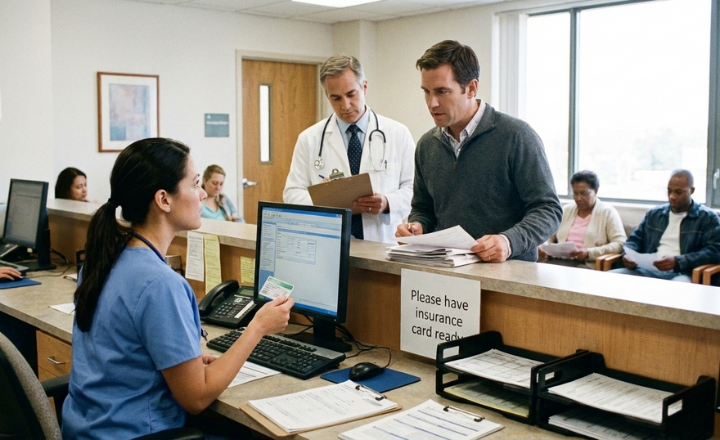
Insurance Eligibility Verification plays a key role in confirming coverage before services are delivered. This checklist outlines the essential steps front desk teams should follow to review insurance details, plan rules, network status, and patient responsibility before check-in, helping reduce coverage issues and improve visit readiness.
Automating Eligibility Verification: How to Stop “Active Policy” Denials Before the Patient Arrives
“Active policy” denials often occur when eligibility is checked only once and not revalidated before the visit. This blog explains how automating eligibility verification helps practices catch coverage changes early, reduce avoidable denials, and prevent delays before the patient even arrives.
How Automating Patient Eligibility Reduces Front-End Denials and Speeds Up Claim Approvals
Front-end claim denials drain revenue and slow down reimbursements. This guide explains how automating patient eligibility checks can prevent errors, improve claim success rates, and streamline your healthcare billing process.
Why Patient Eligibility Verification Is Important Before Every Appointment
Patient Eligibility Verification before every visit helps prevent billing issues, claim denials, and ensures smoother operations for both patients and providers.
Eligibility Verification in the Revenue Cycle: How It Improves Patient Experience
Eligibility verification in the revenue cycle is more than paperwork—it’s key to preventing surprise bills, reducing denials, and improving the overall patient experience.
Benefit Verification in Medical Billing with This Step-by-Step Guide
Benefit verification in medical billing is the first step to avoiding denials and delayed payments. This blog walks you through the process, common errors, and how automation and outsourcing can improve accuracy and patient experience.
Demystifying the Eligibility Verification Process for Front Desk Teams
Front desk teams are the first defense against claim denials. Explore a step-by-step eligibility verification workflow to improve accuracy and patient trust.
How to Improve Eligibility Verification & Prior Authorization in Medical Billing
Not sure when or how to verify coverage or get approvals? This article simplifies it all with real-world tips and tools.
Common Eligibility Verification Mistakes (and How to Avoid Them)
From skipped re-verification to poor documentation, eligibility mistakes cost providers revenue and patient trust. Here’s how to prevent denials.