The Revenue Cycle Blog
Filter By
- ABA Therapy Billing
- AI in Medical Billing
- AI in Revenue Cycle
- Accounts Receivable Management
- Accounts Receivable Mangement
- Allergy and Immunology Billing Services
- Anesthesia Billing Services
- Back Office Revenue Cycle
- Bariatric Surgery Billing
- Billing For Physician Practice and Medical Groups
- Billing for Physician Practices and Medical Groups
- Blog
- COVID-19 Billing
- CPT Codes
- Cardiology Billing Services
- Charge Capture Services
- Charge Entry - Medical Billing
- Charge Entry Services
- Clinical Documentation Improvement - CDI
- Clinical Documentation Integrity
- Company News
- Credit Balance Services
- DME Billing Services
- Denial Code CO-97
- Denial Management - Medical Billing
- Dermatology Billing Services
- E&M
- Electronic Health Records
- Eligibility and Benefits Verification Services
- Emergency Department Billing Services
- FAQs
- Family Practice Billing Services
- G Code
- Gastroenterology Billing Services
- General Surgery Billing Services
- HCC Coding
- HCC Coding Services
- HCPCS
- Healthcare Collections
- Hospitals
- Internal Medicine Billing Services
- Medical Billing Company
- Medical Billing Services
- Medical Billing Services in California
- Medical Billing Services in Texas
- Medical Claim Submission
- Medical Coding Services
- Mental Health Billing Services
- Mental health Billing Services
- Mid Cycle in Revenue Cycle
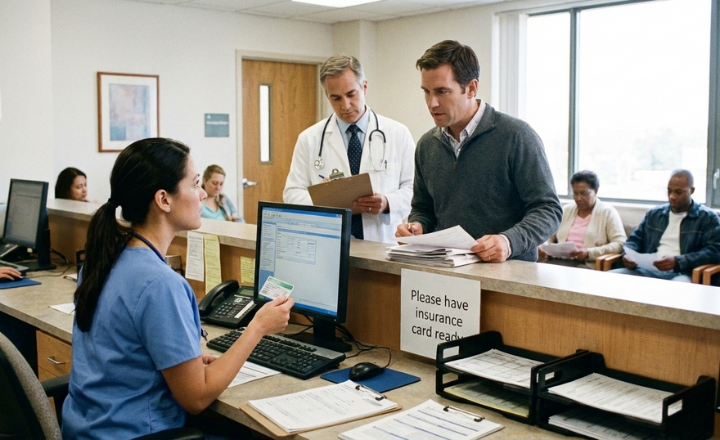
Patient Insurance Verification: What Happens When You Skip It?
Skipping patient insurance verification can lead to denied claims, delayed payments, and increased follow-up work weeks after a visit. This blog explains how missed verification affects billing, scheduling, and front desk workflows, and outlines the common challenges healthcare practices face when insurance details are not confirmed in advance.
Medical Billing Services Cost in the USA: Solo Practice vs. Hospital
Medical billing services cost in the USA varies widely between solo practices and hospitals. This guide breaks down pricing factors, cost ranges, and how providers can optimize billing expenses.
How Insurance Verification Improves Patient Intake Efficiency for Multi-Location Clinics
Insurance verification helps improve patient intake efficiency for multi-location clinics by reducing intake delays and shortening check-in time. This blog explains how early verification, standardized processes, and automation support consistent patient flow across multiple clinic locations.
How Insurance Eligibility Verification Services Prevent Same-Day Claim Rejections
Same-day claim rejections often occur due to eligibility issues identified too late in the billing process. This blog explains how Insurance Eligibility Verification Services help prevent these rejections by validating insurance details before claims are created, reducing errors, rework, and delays in claim processing.
How To Verify Patient Insurance Eligibility Verification
Patient insurance eligibility verification involves reviewing coverage status, benefits, network participation, and payer requirements before services are provided. This blog explains key verification checks that support accurate scheduling decisions and billing preparation.
Insurance Eligibility Verification Checklist Every Front Desk Should Use
Insurance Eligibility Verification plays a key role in confirming coverage before services are delivered. This checklist outlines the essential steps front desk teams should follow to review insurance details, plan rules, network status, and patient responsibility before check-in, helping reduce coverage issues and improve visit readiness.
5 Ways to Speed Up Prior Authorization for Biologics and Infusions
Biologics and infusion therapies often face complex prior authorization requirements. Discover practical ways to streamline documentation, accelerate approvals, and reduce administrative burden.
Claims Submission in Medical Billing Explained: From Patient Intake to Payment
Claims submission in medical billing follows a defined path from patient intake to payment. Each step—eligibility checks, documentation, coding, claim submission, and payer review—guides how claims move through the billing cycle until payment is posted and patient balances are billed.
How to Choose the Best Gastroenterology EMR with Integrated Billing
Choosing the right Gastroenterology EMR with Integrated Billing can significantly improve documentation accuracy, reduce billing errors, and accelerate revenue cycle performance for GI practices.
8 Important Rules for Paper Claim Submission in Medical Billing Using the CMS-1500 Form
Paper claim submission in medical billing remains necessary for certain payers and claim types. CMS-1500 forms require strict rules for formatting, data entry, and handling. Small errors can result in claim returns or delays. This blog outlines key CMS-1500 rules that help reduce paper claim issues and improve processing.
Types of Claim Submission in Medical Billing You Must Get Right the First Time
Understanding claim submission types in medical billing helps determine how claims are reviewed and processed by insurance payers. This blog covers the key submission methods, purposes, and formats, and explains how selecting the right approach from the start can reduce delays and limit follow-up activity throughout the billing cycle.
Automating Eligibility Verification: How to Stop “Active Policy” Denials Before the Patient Arrives
“Active policy” denials often occur when eligibility is checked only once and not revalidated before the visit. This blog explains how automating eligibility verification helps practices catch coverage changes early, reduce avoidable denials, and prevent delays before the patient even arrives.
5 Signs Your Patient Registration Process is Causing Downstream Claim Rejections.
Claim rejections often begin long before billing—during patient registration. Learn five signs your patient registration process is causing claim rejections and how front-end fixes improve clean claim rates and revenue flow.
Top 10 Best Cardiology Billing Services in the US
Cardiology billing is complex and high risk. Explore the top 10 best cardiology billing services in the US and learn how specialty RCM improves reimbursements and reduces denials.
Top 10 Best Mental Health Billing Services in US
Choosing the right mental health billing partner is critical for reducing denials and maximizing revenue. Explore the top 10 best mental health billing services, with expert insights into behavioral health RCM and billing performance.
Accounts Receivable Management Services in Florida: What Clinics Do Right
Florida clinics succeed in managing claims, follow-ups, and denials through structured AR practices. Timely submissions and weekly aging reviews ensure smoother billing, faster reimbursements, and consistent revenue, showing what Florida clinics get right with Accounts Receivable Management Services in Florida.
How Accounts Receivable and Denial Management Services Reduce A/R Days for Specialty Practices
Specialty practices often face delayed payments due to missed follow-ups and unresolved claim denials. A structured approach to claim tracking and denial resolution helps reduce A/R days by addressing unpaid and denied claims early. This blog explains how coordinated A/R and denial management improves reimbursement timelines and keeps billing workflows on track.
The Cost of Manual Prior Authorizations: Is Your Staff Spending Too Much Time on the Phone?
Manual prior authorizations affect staff productivity, registration accuracy, and claim outcomes. Explore their impact on healthcare revenue cycles.
How Clinical Psychology Billing Management Reduces 90837 Claim Rejections
90837 claim denials can disrupt cash flow for psychology practices. Documentation gaps and payer rules often lead to rejected claims and delays. This blog explains how clinical psychology billing management helps reduce rejections, strengthen compliance, and support more consistent reimbursements.
Why is my EOB Payment Posting Not Matching Insurance Payments?
EOB payment posting mismatches can lead to incorrect balances, delayed follow-up, and reporting issues. This blog explains why posted payments don’t match insurance remittances and how to identify and fix common posting errors early.