The Revenue Cycle Blog
Filter By
- ABA Therapy Billing
- AI in Medical Billing
- AI in Revenue Cycle
- Accounts Receivable Management
- Accounts Receivable Mangement
- Allergy and Immunology Billing Services
- Anesthesia Billing Services
- Back Office Revenue Cycle
- Bariatric Surgery Billing
- Billing For Physician Practice and Medical Groups
- Billing for Physician Practices and Medical Groups
- Blog
- COVID-19 Billing
- CPT Codes
- Cardiology Billing Services
- Charge Capture Services
- Charge Entry - Medical Billing
- Charge Entry Services
- Clinical Documentation Improvement - CDI
- Clinical Documentation Integrity
- Company News
- Credit Balance Services
- DME Billing Services
- Denial Code CO-97
- Denial Management - Medical Billing
- Dermatology Billing Services
- E&M
- Electronic Health Records
- Eligibility and Benefits Verification Services
- Emergency Department Billing Services
- FAQs
- Family Practice Billing Services
- G Code
- Gastroenterology Billing Services
- General Surgery Billing Services
- HCC Coding
- HCC Coding Services
- HCPCS
- Healthcare Collections
- Hospitals
- Internal Medicine Billing Services
- Medical Billing Company
- Medical Billing Services
- Medical Billing Services in California
- Medical Billing Services in Texas
- Medical Claim Submission
- Medical Coding Services
- Mental Health Billing Services
- Mental health Billing Services
- Mid Cycle in Revenue Cycle
The Cost of Manual Prior Authorizations: Is Your Staff Spending Too Much Time on the Phone?
Manual prior authorizations affect staff productivity, registration accuracy, and claim outcomes. Explore their impact on healthcare revenue cycles.
How Clinical Psychology Billing Management Reduces 90837 Claim Rejections
90837 claim denials can disrupt cash flow for psychology practices. Documentation gaps and payer rules often lead to rejected claims and delays. This blog explains how clinical psychology billing management helps reduce rejections, strengthen compliance, and support more consistent reimbursements.
Why is my EOB Payment Posting Not Matching Insurance Payments?
EOB payment posting mismatches can lead to incorrect balances, delayed follow-up, and reporting issues. This blog explains why posted payments don’t match insurance remittances and how to identify and fix common posting errors early.
What Is Payment Posting in Medical Billing? Process, Importance & Best Practices
Payment posting is a key step in medical billing that reflects how insurance and patient payments are recorded after claims are processed. This blog explains what payment posting in medical billing involves, outlines the step-by-step process, highlights its importance in billing workflows & shares best practices to help healthcare providers manage payments and follow-ups more effectively.
Payment Posting in Medical Billing for Zero Payment and Denied EOBs
Payment posting in medical billing plays a key role when EOBs show zero payment or claim denials. This blog explains how unpaid EOBs are posted, reviewed, and moved forward for correction or appeal.
Why Insurance Claims Still Unpaid After 60 Days in A/R Billing & Follow Up?
Insurance claims unpaid after 60 days signal deeper issues within A/R Billing & Follow Up. This blog breaks down why claims remain unresolved, how payer delays and workflow gaps contribute to aging, and what clinics can do to reduce long-outstanding balances.
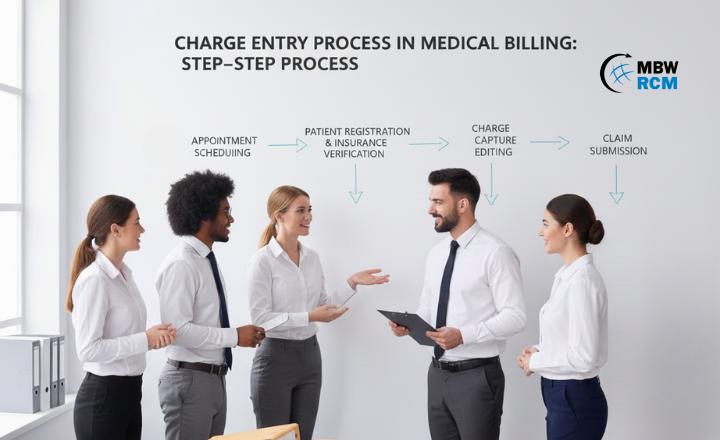
Charge Entry Process in Medical Billing: Step-by-Step Process
The charge entry process in medical billing converts patient services into billable charges. This guide explains each step, required documents, common challenges, and best practices to support clean claim creation.
Role of Effective Billing in Orthopedic Practice Revenue
Effective billing plays a major role in revenue performance for orthopedic practices. From accurate coding and streamlined claim submission to stronger patient collections, each step influences how smoothly payments flow. This blog breaks down how structured billing systems reduce errors, support compliance, and help orthopedic teams maintain steady, predictable income while improving overall practice operations.
Facility vs. Physician: Clarifying the Most Confusing Rules in Emergency Department Billing
Confused about the difference between facility and physician billing in the Emergency Department? This guide breaks down the rules, audit risks, and best practices that impact compliant ED billing and reimbursement.
Bundled Payments (BPCI Advanced): An Orthopedic Practice's Strategy for Max Revenue
Bundled Payments (BPCI Advanced) are reshaping orthopedic reimbursement by rewarding coordinated, episode-based care. Learn how practices can improve margins, manage risk, and succeed in value-based care.
Top 10 Orthopedic Billing Company in the USA
Choosing the right orthopedic billing company in the USA can directly impact your practice’s revenue and compliance. This guide explains how to evaluate orthopedic billing partners, reduce denials, and optimize collections for your specialty.
10 Reasons Outsourced Orthopedic Coding Solutions Outperform In-House Teams
Outsourced orthopedic coding solutions offer a powerful alternative to in-house teams by improving coding accuracy, reducing denials, and strengthening compliance. This blog compares both approaches to help orthopedic practices choose the right coding strategy for long-term revenue performance.
Prior Authorization Outsourcing: How to Reduce Peer-to-Peer Reviews by 40%
Peer-to-peer reviews delay care and disrupt workflows. Discover how prior authorization outsourcing reduces unnecessary reviews and improves authorization approvals.
How Counseling and Therapy Reimbursement Services Resolve Underpaid Claims
Underpaid claims can impact a practice’s revenue, but Counseling and Therapy Reimbursement Services help identify discrepancies, correct claim issues, and recover missing payments. With targeted audits and strategic appeals, these services support a stronger and more reliable reimbursement process.
6 Best Ways to Improve Behavioral Health Revenue Cycle Management Results
Behavioral Health Revenue Cycle Management plays a major role in how smoothly a practice operates. In this guide, you’ll explore 6 best ways to strengthen claim outcomes, reduce delays, and improve overall billing performance. Each method offers practical steps your team can use to achieve more reliable and consistent revenue cycle results.
Escape Billing Burnout Using Mental Health Practice Billing Support
Billing burnout is a growing challenge for many mental health practices managing complex payer requirements and ongoing claim demands. With structured Mental Health Practice Billing Support, organizations can stabilize workflows, reduce administrative strain, and maintain stronger focus on delivering quality client care.
How to Handle Increased No-Shows in Telehealth Mental Health Billing Services
Rising no-shows impact the flow of telehealth mental health practices. Learn how effective billing workflows, communication habits, tech readiness, and reminder systems help reduce missed appointments and support smoother virtual care.
Linking EMR and Outpatient Therapy Billing Solutions for Clean Claims
Linking your EMR with Outpatient Therapy Billing Solutions can transform how your therapy practice manages claims. By optimizing documentation and reducing errors, integrated systems help PT, OT, and Speech Therapy clinics achieve cleaner claims and faster reimbursements.
Top 5 RCM Automation Tools That Reduce Claim Submission Errors
Minimizing claim submission errors is important for maintaining steady reimbursements. Manual workflows often miss coding details, eligibility changes, and payer rules. RCM automation tools help address these issues with structured validation and real-time checks. This overview highlights five tools that improve submission quality, reduce denials, and support more consistent billing results.
How Cardiac Diagnostic Billing Experts Ensure You Get Paid for Every Procedure
Cardiology practices lose revenue when diagnostic tests are missed or claims are rejected. Cardiac Diagnostic Billing Experts support precise coding, documentation review, and payer-rule compliance to help ensure each diagnostic service is billed correctly and reimbursed on time.