Charge Entry Process in Medical Billing: Step-by-Step Process
The charge entry process in medical billing is the stage where services provided during a patient visit are converted into billable charges. In simple terms, it translates clinical documentation into structured data that billing systems can process. The medical billing charge entry process connects encounter forms, procedure codes, diagnosis codes, and charge amounts into one workflow. Without a reliable charge entry billing process, claims cannot move forward in the revenue cycle. This step plays a direct role in how services are communicated to payers.
Table of Contents
Importance of Charge Entry Process in Medical Billing
Charge entry in medical billing is important because it records what service was performed, why it was performed, who performed it, and how much to bill. This stage includes entering CPT codes, linking ICD diagnoses, applying modifiers, assigning providers, and adding charge amounts. A well-handled charge entry process medical billing reduces claim edits, limits follow-ups, and keeps the charge entry process in RCM moving without disruption, directly affecting how claims progress. Learn more about why charge entry in medical billing matters.
Documents Used in Charge Entry Billing Process
The charge entry billing process depends on specific documents that support accurate billing and claim creation. In charge entry in healthcare billing, each document plays a defined role in building a complete charge record.
Encounter forms – list services performed during the visit
Provider progress notes – justify medical necessity
Patient demographic and insurance records – support payer identification
Fee schedules – guide charge amount entry
Missing documents slow the medical billing charge entry process.
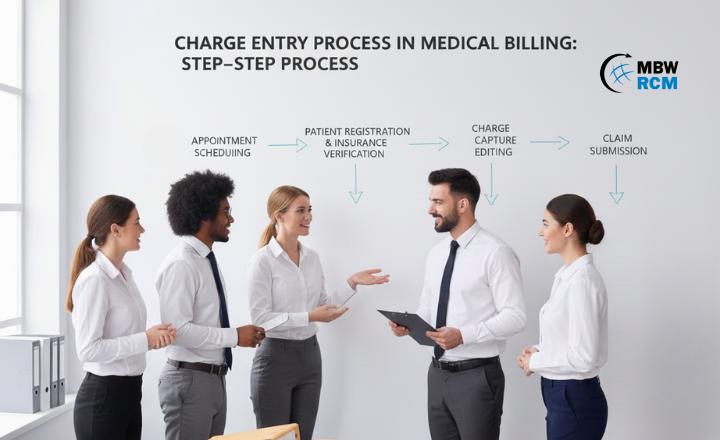
Step-by-Step Charge Entry Process in Medical Billing
Before the charge entry process begins, billing teams organize patient visit information to make sure every service provided is captured and billed correctly. The charge entry process in medical billing is not a single task but a series of checks and entries that confirm documentation, codes, charges, and provider details. Understanding this flow helps practices identify where errors occur and how charge entry supports clean claim creation.
Receipt of Patient Encounter Documentation
The charge entry process in medical billing begins when patient encounter documentation is received from providers or EHR systems. These records include dates of service, procedures performed, and provider details. In charge entry in RCM, timely receipt of encounter forms ensures services are not missed. Delays at this stage often slow the medical billing charge entry process and impact downstream billing activities.
Review of Medical Records for Billable Services
During this step, billing staff review medical records to identify all billable services. The medical billing charge entry process depends on confirming procedures, units, and supplies documented by providers. Incomplete or unclear records require clarification before proceeding. Proper review supports accurate charge entry procedures in medical billing and prevents missed or duplicated charges.
Patient Demographic Verification
Patient demographic verification is a core part of the charge entry billing process. Details such as patient name, date of birth, and insurance ID are checked against records. In charge entry process medical billing, incorrect demographics often lead to claim rejections. Verifying this information early helps maintain a steady charge entry process in RCM.
Insurance and Coverage Confirmation
Insurance verification confirms active coverage, payer type, and plan details. In charge entry in medical billing, this step aligns services with the correct insurance policy. Coverage issues identified early prevent unnecessary rework. A consistent charge entry process in RCM relies on accurate insurance data before charges are entered into billing systems.
Assignment and Validation of CPT/HCPCS Codes
CPT and HCPCS codes are assigned or validated to represent services provided. In the medical billing charge entry process, these codes translate clinical care into standardized billing language. Incorrect coding affects reimbursement and claim acceptance. Validating codes during charge entry ensures consistency across the charge entry billing process.
Diagnosis Code (ICD-10) Linking
Diagnosis codes are linked to procedures to support medical necessity. In charge entry procedures in medical billing, each CPT code must connect to an appropriate ICD-10 code. Incorrect linking often leads to payer edits and delays. When diagnosis-to-procedure linking is incorrect, claims are often returned for correction, which is why billing teams follow specific steps to fix diagnosis-related charge entry errors in medical billing and keep the charge entry process aligned with documented conditions.
Application of Modifiers and Units
Modifiers and units clarify how services were delivered. In charge entry process medical billing, modifiers explain multiple procedures, repeat services, or special circumstances. Units define quantity or duration. Missing modifiers or incorrect units are common issues in charge entry in healthcare billing and may result in partial payments.
Charge Amount Entry Using Fee Schedules
Charge amounts are entered using fee schedules or chargemaster data. The medical billing charge entry process relies on standardized pricing to maintain consistency. Entering correct charge values supports predictable billing outcomes. This step is essential within the charge entry process in RCM to align services with defined rates.
Provider and Place of Service Assignment
Provider details and place-of-service codes identify who performed the service and where it occurred. In charge entry in medical billing, incorrect provider mapping can delay claims. Assigning accurate details supports payer processing and keeps the charge entry billing process aligned with documentation.
Entry of Charges Into Billing System
All validated data is entered into the billing or practice management system. This includes codes, demographics, modifiers, provider details, and charge values. In charge entry process medical billing, system entry converts reviewed data into claim-ready records. Errors at this stage often require time-consuming corrections.
Internal Charge Review and Validation
Before claims move forward, charge entries undergo internal review. This step checks for missing fields, incorrect code links, and duplicate entries. In the medical billing charge entry process, internal validation reduces downstream claim edits and rework. A strong review step supports stable charge entry solutions in medical billing.
Release of Charges for Claim Creation
Once reviewed, charges are released for claim generation. At this stage, the charge entry process in RCM hands off data to claims processing. Clean charge entry allows claims to proceed without delay. This final step completes the charge entry process in medical billing and prepares data for submission.
Charge Entry in Medical Billing Process Workflow:
Common Challenges in Medical Billing Charge Entry Process
The medical billing charge entry process faces several challenges. Incomplete encounter forms delay data entry. Incorrect diagnosis linking can cause payer edits. Manual entry increases the chance of missing modifiers or mismatched codes. In high-volume practices, backlogs may form if charge entry is not performed daily. These challenges show why a structured charge entry process in RCM is necessary to keep billing operations running smoothly. For more insights on how to optimize charge entry in medical practices.
Charge Entry Process in Medical Billing vs Charge Capture
The charge entry process in medical billing is often confused with charge capture, but they serve different purposes. Charge capture records services at the point of care, usually by providers. Charge entry takes that captured information and inputs it into billing systems. In other words, capture happens during the visit, while charge entry happens afterward. The charge entry process medical billing depends heavily on how well charge capture is performed. Read more about the difference between charge capture and charge entry.
Specialty-Based charge entry process in RCM
The specialty-based charge entry process in medical billing changes based on how services are reported and billed. Each specialty follows specific rules that billing teams must recognize during charge entry.
Primary care – E/M level selection and preventive services
Surgical specialties – global periods, bundled procedures, and modifiers
Radiology – technical and professional component billing
Laboratory services – panel codes and individual test mapping
Specialty knowledge strengthens charge entry procedures in medical billing.
Outsourced Charge Entry Services for Healthcare Providers
Many practices turn to outsourced charge entry medical billing services to manage workload and volume. Outsourcing allows healthcare providers to send encounter data to trained billing teams who handle charge input and validation. These charge entry solutions in medical billing help practices maintain consistency without expanding internal staff. For providers with high claim volume or limited billing resources, outsourcing supports steady charge entry operations.
Finding the Right Charge Entry Partner: Why MBW RCM!
Choosing the right partner for outsourced charge entry medical billing requires experience and process knowledge. MBW RCM supports healthcare providers with structured charge entry solutions in medical billing tailored to practice needs. Our team supports documentation review, charge entry execution, and internal validation to help keep billing operations on track. For practices seeking dependable support, MBW RCM offers scalable charge entry services aligned with revenue cycle goals.
Final Takeaway
The charge entry process in medical billing forms the foundation of every insurance claim. From documentation review to charge validation, each step influences how services are billed and processed. By understanding the medical billing charge entry process and applying best practices—or working with experienced partners—healthcare providers can maintain steady billing workflows and reduce operational friction.
FAQs: Charge Entry in Medical Billing
Request for Information
A well-structured charge entry process is a key part of efficient medical billing. Complete the form below to receive guidance on improving charge entry workflows, reducing data gaps, and supporting smoother claim processing. Our team can help your practice strengthen charge entry operations and maintain consistent billing outcomes across your revenue cycle.