Gastroenterology Billing: Screening vs Diagnostic Colonoscopies
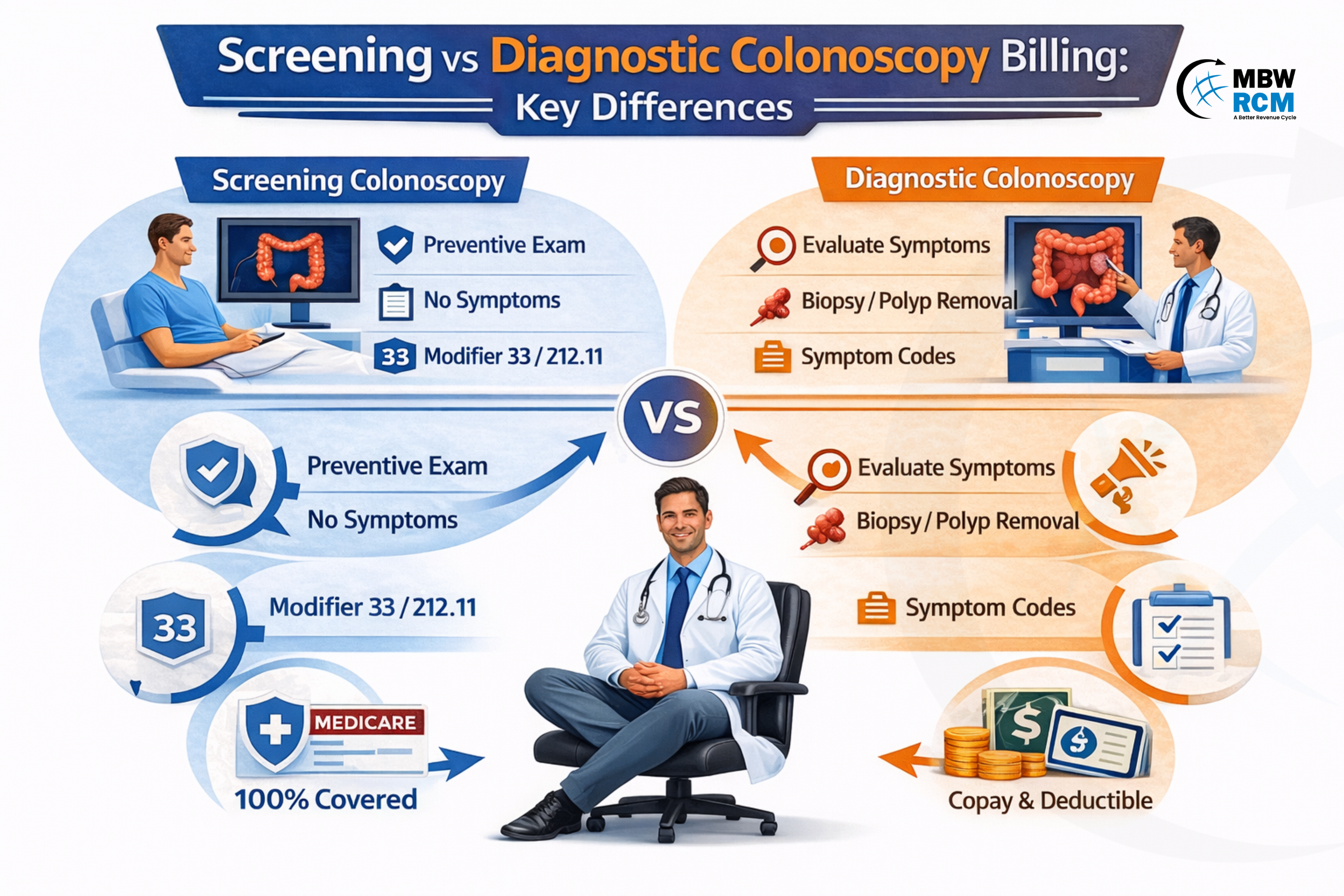
Colonoscopy billing varies depending on whether the procedure is performed for screening or diagnostic purposes. This distinction is important in Gastroenterology Billing because it affects coding, insurance coverage, and reimbursement.
Understanding the difference helps providers and billing teams use the correct codes and avoid claim denials. This blog explains the key billing differences between screening and diagnostic colonoscopies, including coding requirements and common errors, to ensure proper and efficient billing.
Table of Contents
Screening Colonoscopy
A screening colonoscopy is performed for preventive purposes when the patient has no gastrointestinal symptoms. The goal is early detection of colorectal cancer or precancerous lesions.
From a screening colonoscopy billing perspective, preventive colonoscopies are typically recommended:
Every 10 years for average-risk patients aged 45 and older
Every 5 years for high-risk patients (family history or prior polyps)
Based on payer-specific preventive guidelines
Screening procedures are classified under preventive care and billed accordingly within structured Gastroenterology Billing systems supported by efficient GI billing services.
For example, if a 50-year-old asymptomatic patient undergoes routine colon cancer screening, the procedure is billed as screening, even if polyps are discovered during the procedure.
Screening procedures play a vital role in preventive care and are a core component of modern gastroenterology medical billing operations.
Diagnostic Colonoscopy
A diagnostic colonoscopy is performed when the patient presents with symptoms, abnormal lab results, or a known gastrointestinal condition.
Common indications include:
Rectal bleeding
Iron deficiency anemia
Chronic diarrhea lasting more than 14 days
Abdominal pain
Positive FIT or stool test
From a diagnostic colonoscopy billing standpoint, these procedures are classified as medically necessary diagnostic services rather than preventive services.
Unlike screening procedures, diagnostic colonoscopies often involve condition-specific evaluation, biopsy, or therapeutic intervention, which affects CPT selection and reimbursement within the colonoscopy billing and coding framework and overall Gastroenterology Billing accuracy.
Key Differences Between Screening and Diagnostic Colonoscopy
Understanding the billing distinction is essential for accurate reimbursement and compliance in Gastroenterology Billing. The classification affects how payers process claims, determine preventive eligibility, and assign patient financial responsibility.
Proper identification ensures the correct use of CPT codes, diagnosis codes, and modifiers, which directly impacts claim approval and payment timelines.The following table highlights the key billing and coverage differences between screening and diagnostic colonoscopy procedures:
These differences directly affect the GI billing claim process, reimbursement timelines, and patient billing outcomes.
Colonoscopy Classification Based on Medical Necessity
Medical necessity is the primary factor used by insurance providers to determine colonoscopy classification.
⇒ Screening Colonoscopy – It is classified as preventive because it is performed without symptoms.
⇒ Diagnostic Colonoscopy – It is classified as medically necessary because it is performed to evaluate specific conditions or symptoms.
This classification impacts reimbursement timelines and is closely monitored through gastroenterology revenue cycle management workflows, where accurate procedure classification helps reduce claim denials and improves payment turnaround within 14–30 days, strengthening overall Gastroenterology Billing efficiency.
CPT Coding for Screening & Diagnostic Colonoscopy Billing
CPT code selection depends on the procedure performed and whether intervention occurred.
Common colonoscopy CPT codes billing examples include:
45378 – Diagnostic colonoscopy without intervention
45380 – Colonoscopy with biopsy
45385 – Colonoscopy with snare removal of polyp
Medicare also uses:
G0121 – Screening colonoscopy for average-risk patients
G0105 – Screening colonoscopy for high-risk patients
These codes are part of standard GI procedure billing codes and must be selected accurately to ensure proper reimbursement using correct cpt codes for gastroenterology.
Correct CPT usage is essential in Gastroenterology Billing to prevent claim rejections and delays.
ICD-10 Coding Requirements for Colonoscopy Procedures
Diagnosis coding determines whether a colonoscopy is classified as screening or diagnostic.
Screening colonoscopy diagnosis codes include:
Z12.11 – Encounter for screening for malignant neoplasm of colon
Diagnostic colonoscopy diagnosis codes include:
K62.5 – Rectal bleeding
D50.9 – Iron deficiency anemia
R19.4 – Change in bowel habits
Proper diagnosis coding ensures proper claim processing and reduces denials within modern GI Billing workflows. Want to know how optimized gastroenterology RCM can reduce accounts receivable days and improve reimbursement timelines? Discover the strategies that helped reduce GI A/R by 42 days here:
Modifier Usage in Gastroenterology Billing for Colonoscopy
Modifiers are used to indicate preventive intent when therapeutic intervention occurs during screening procedures.
Common colonoscopy billing modifiers include:
Modifier 33 – Preventive service modifier (commercial insurance)
Modifier PT – Screening converted to diagnostic (Medicare)
Incorrect modifier usage is one of the most common causes of claim denial and delayed reimbursement, affecting the overall performance of GI Billing and revenue cycle operations.
Billing for Screening Colonoscopy Converted to Diagnostic
A screening colonoscopy may require biopsy or polyp removal during the procedure.
In such cases:
CPT code reflects intervention performed
Screening diagnosis remains primary
Modifier 33 or PT must be appended
This scenario is common, occurring in approximately 35–40% of preventive colonoscopy procedures.
Proper handling of conversion cases ensures accurate reimbursement and prevents claim reprocessing delays within structured Gastroenterology Billing workflows. For official Medicare billing and modifier guidelines, refer to the CMS preventive colonoscopy conversion billing requirements:
Insurance and Medicare Coverage for Colonoscopy Billing
Insurance coverage varies based on classification. Screening colonoscopies are typically covered under preventive benefits, while diagnostic colonoscopies are processed under medical necessity benefits and may include copay, coinsurance, or deductible based on the patient’s insurance plan.
Medicare preventive screening frequency:
Every 120 months (10 years) for average risk
Every 24 months (2 years) for high risk
Commercial insurance typically follows preventive care mandates under ACA guidelines.
Proper payer-specific coding helps improve reimbursement efficiency and supports overall best gastroenterology rcm performance metrics and optimized gastroenterology revenue cycle management.
Common Billing Errors in GI Billing for Colonoscopy
Colonoscopy billing errors are a major cause of claim denials and delayed payments, directly affecting Gastroenterology Billing performance. GI procedures account for nearly 20–25% of total gastroenterology claims, and coding errors can delay reimbursement by 30–60 days, increasing administrative workload and revenue cycle inefficiencies.
Preventive vs Diagnostic Misclassification
Incorrect classification of screening colonoscopy as diagnostic due to wrong ICD-10 coding (instead of Z12.11) can result in claim denial or incorrect reimbursement. This error affects preventive coverage eligibility and delays payment by 15–30 days.
Missing Preventive Modifiers
Failure to append Modifier 33 or Modifier PT when screening colonoscopy converts to therapeutic intervention can cause claims to process incorrectly. Modifier errors contribute to approximately 12–14% of colonoscopy denials.
Incorrect CPT Code Selection
Using incorrect CPT codes or mismatching procedure documentation with billed services can result in underpayment, claim rejection, or payer review. Accurate CPT selection ensures proper reimbursement and faster claim processing.
Revenue Cycle and Documentation Impact
Incomplete medical necessity documentation increases denial risk and delays reimbursement. These errors negatively impact Gastroenterology KPIs, including clean claim rate and A/R days.
Proper coding workflows and experienced Gastroenterology Billing Company support help reduce billing errors, improve claim accuracy, and ensure faster reimbursement while strengthening overall revenue cycle performance.
Conclusion
Proper classification of screening and diagnostic colonoscopies is essential to ensure appropriate reimbursement, avoid claim denials, and maintain compliance. Using the right CPT codes, ICD-10 codes, and modifiers helps improve claim acceptance and supports efficient gastroenterology billing and coding workflows.
If your practice needs expert support to improve billing accuracy and reduce denials, our team is here to help. Contact MBW RCM today to streamline your billing process and optimize your revenue cycle.
FAQs: Screening vs Diagnostic Colonoscopy Billing
Request for Information
Facing screening vs diagnostic colonoscopy billing challenges, coding errors, modifier issues, or claim denials? A gastroenterology billing expert can review your workflows and identify improvement areas.
Fill out the form below to connect with a specialist and improve your gastroenterology billing efficiency and reimbursement performance.