How Gastroenterology RCM Reduced A/R by 42 Days: Explained
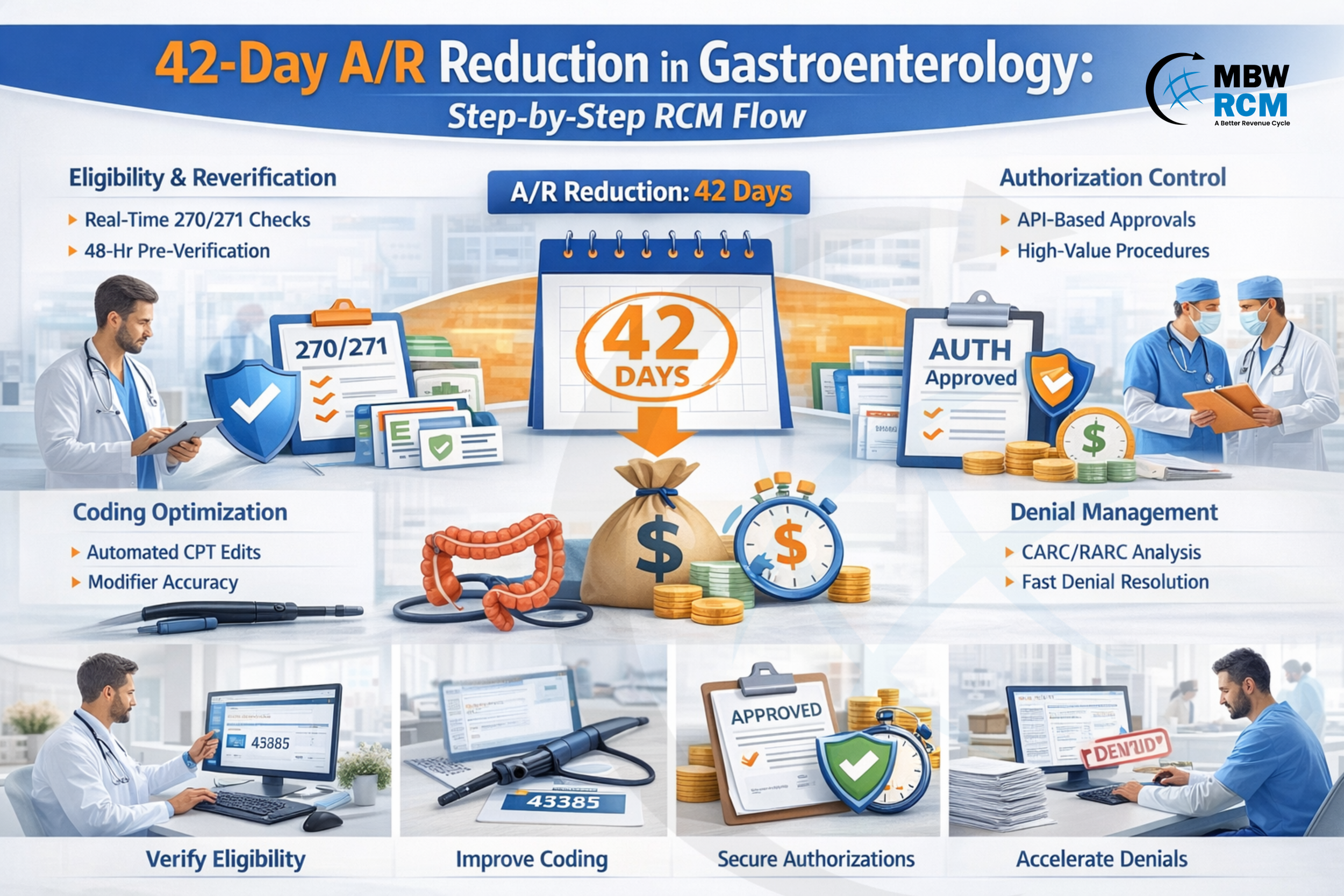
Reducing Accounts Receivable (A/R) days is a top financial priority for gastroenterology practices, where procedure-based revenue and payer requirements directly affect payment timelines. When A/R increases, it impacts cash flow and revenue predictability. Achieving a 42-day reduction in A/R requires targeted improvements designed for gastroenterology billing workflows.
This blog explains how Gastroenterology RCM helped reduce A/R by 42 days through improvements in eligibility verification, coding accuracy, authorization validation, denial management, and claim processing efficiency.
Table of Contents
1. Real-Time 270/271 + 48hr Reverification Protocol
Real-time 270/271 eligibility transactions were deployed during scheduling, along with mandatory re-verification 48 hours before procedures. This workflow is a foundational step in GI Revenue Cycle Optimization and supports payer-ready claims before encounter completion.
This specifically prevented:
COB conflicts in Medicare secondary GI claims
Plan switching errors in colonoscopy preventive coverage
Deductible reset errors at procedure month
A/R Reduction Outcome:
Clean claim rate increased from 82% → 96%, eliminating ~18–22 days of rework lag. This directly supports Clean Claim Rate Improvement initiatives and strengthens Gastroenterology RCM front-end revenue protection models.
2. CPT 45378–45385 Modifier Logic Automation
The approach used GI-specific coding edit logic targeting high-volume colonoscopy CPT bands. Accurate handling of Gastroenterology CPT Codes is essential for payer adjudication accuracy and supports high procedural claim acceptance.
Automated checks validated:
Screening → Diagnostic conversion triggers
-PT modifier for Medicare screening conversions
-59 / XS distinct procedural service conflicts
Add-on therapeutic CPT bundling edits
A/R Reduction Outcome:
Procedure coding denials dropped 61%, removing ~9–12 A/R days from appeals. This is a direct driver of Denial Rate Reduction in Medical Billing and strengthens procedural coding accuracy within Gastroenterology RCM workflows.
3. LCD/NCD Auto-Flagging Using Dx–CPT Mapping
Dx-to-CPT medical necessity rule mapping was implemented and aligned to payer LCD/NCD libraries. This mapping approach supports documentation-driven claim acceptance across Gastroenterology Billing Services workflows.
Pre-bill claim scrubbing identified missing:
Alarm symptom documentation
Failed conservative therapy
Risk factor ICD linkage
A/R Reduction Outcome:
Medical necessity denials reduced 58%, eliminating long 30–45 day appeal cycles. This contributes significantly to Reduce AR Days in Medical Billing initiatives and supports measurable Gastroenterology RCM KPIs tied to denial prevention.
4. 72hr Pre-Service Auth Status API Pulls
Instead of manual portal checks, automated authorization status pulls were executed using payer APIs. This process supports scalable AR Days Reduction in Healthcare RCM through real-time payer visibility.
Applied to high-value GI services:
Capsule endoscopy
Biologic infusion J-code therapies
Advanced endoscopic procedures
A/R Reduction Outcome:
Auth-related denials dropped ~70%, accelerating high-dollar reimbursements by ~14–18 days. This level of automation is frequently delivered by a Best Gastroenterology Billing Company operating advanced specialty authorization workflows under Gastroenterology RCM frameworks.
5. Denial Velocity Model Using CARC/RARC Clusters
A/R work queues were rebuilt using CARC/RARC denial clustering + resolution time modeling. This data-driven approach is widely used in advanced GI Medical Billing Performance Improvement programs.
Priority sequence was:
Eligibility CARC (fastest correction window)
Coding edit RARC clusters
Auth mismatch denials
Medical necessity appeals
If you want to know more about payer guidance and documentation standards, access detailed CMS guidance on Billing and Coding: Gastroenterology CPT® Modifier 59.
A/R Reduction Outcome:
Cash posting velocity increased 27%, reducing aging >60 days significantly. This model supports enterprise-level Gastroenterology RCM denial intelligence and faster recovery cycles.
6. Pathology Linkage Auto-Attach for GI Procedures
LIS data feeds were integrated to auto-attach pathology references when biopsy CPTs were billed with colonoscopy base codes. This supports end-to-end Gastroenterology EMR Billing Integration for documentation-linked claim submission.
This prevented payer holds requiring:
Histopath confirmation linkage
Specimen medical necessity validation
A/R Reduction Outcome:
Regional payer hold releases improved payment TAT by 7–10 days, supporting specialty-focused AR Days Benchmark Healthcare performance targets.
7. Payer Adjudication TAT Predictive Worklists
Predictive payer payment cycle models were built using historical adjudication turnaround time (TAT) data. This predictive modeling is a core layer of advanced Gastroenterology RCM cash acceleration strategy.
Work queues prioritized claims approaching payer processing cutoff windows.
A/R Reduction Outcome:
Reduced “stuck in processing” claims by ~22%, improving mid-cycle cash flow and supporting long-term Healthcare Revenue Cycle Optimization outcomes.
8. ERA Variance Auto-Reconciliation Using 835 Parsing
Automated 835 ERA parsing identified underpayments and silent denials within 24 hours of posting. This automation layer strengthens enterprise Gastroenterology Revenue Cycle Management reporting accuracy.
Immediate corrected claim or reconsideration workflows were triggered.
A/R Reduction Outcome:
Recovered revenue 2–3 weeks faster versus manual variance discovery, supporting measurable AR Days Reduction in Healthcare RCM and stabilizing downstream collections.
How These Changes Combined to Deliver 42-Day A/R Drop
Stacked revenue cycle improvements helped reduce A/R days across the gastroenterology billing workflow. By optimizing eligibility accuracy, coding validation, documentation alignment, authorization control, and denial prioritization together, claim rework was reduced, first-pass acceptance improved, and payer payment timelines accelerated.
The A/R reduction happened through stacked revenue acceleration layers:
Stacked together → Total A/R Reduction: ~42 Days, demonstrating measurable success in gastroenterology revenue cycle performance improvement.
Gastroenterology RCM A/R Reduction Checklist
Use this checklist to systematically identify and eliminate the most common revenue delays that increase A/R days in gastroenterology billing workflows. Each item directly supports faster claim submission, lower denial rates, and shorter payment cycles.
☐ Verify insurance via real-time eligibility (270/271) before scheduling
☐ Re-verify coverage and benefits 24–48 hours before procedures
☐ Confirm prior authorization for high-value GI services
☐ Validate colonoscopy CPT coding and modifier accuracy pre-submission
☐ Ensure Dx–CPT medical necessity alignment per LCD/NCD rules
☐ Run GI-specific claim scrubbing edits before submission
☐ Correct eligibility, coding, and auth denials within 3–5 days
☐ Monitor clean claim rate and denial trends weekly
☐ Post ERA and identify underpayments within 24–48 hours
☐ Review A/R aging weekly and escalate timely filing risks
Want to Reduce Your Gastroenterology A/R Days?
Reducing A/R by 42 days is achievable when revenue cycle processes are aligned with gastroenterology billing workflows. Improving eligibility accuracy, coding validation, authorization control, and denial resolution can help accelerate payments and improve revenue stability.
Partnering with expert Gastroenterology Billing Services can help maintain lower A/R days and improve claim accuracy. To optimize your GI revenue cycle and accelerate reimbursements, Contact Us to learn how specialized billing support can help improve your financial performance.
FAQs: Gastroenterology Revenue Cycle A/R Management
Request for Information
Facing gastroenterology billing challenges such as eligibility errors, authorization delays, coding issues, or GI claim denials? A billing expert can review your workflows and identify opportunities to reduce A/R days.
Fill out the form below to connect with an MBW RCM specialist to discuss reducing A/R days and improving your gastroenterology billing performance.