Top 20 CPT Codes for Gastroenterology Clinics (2026 Guide)
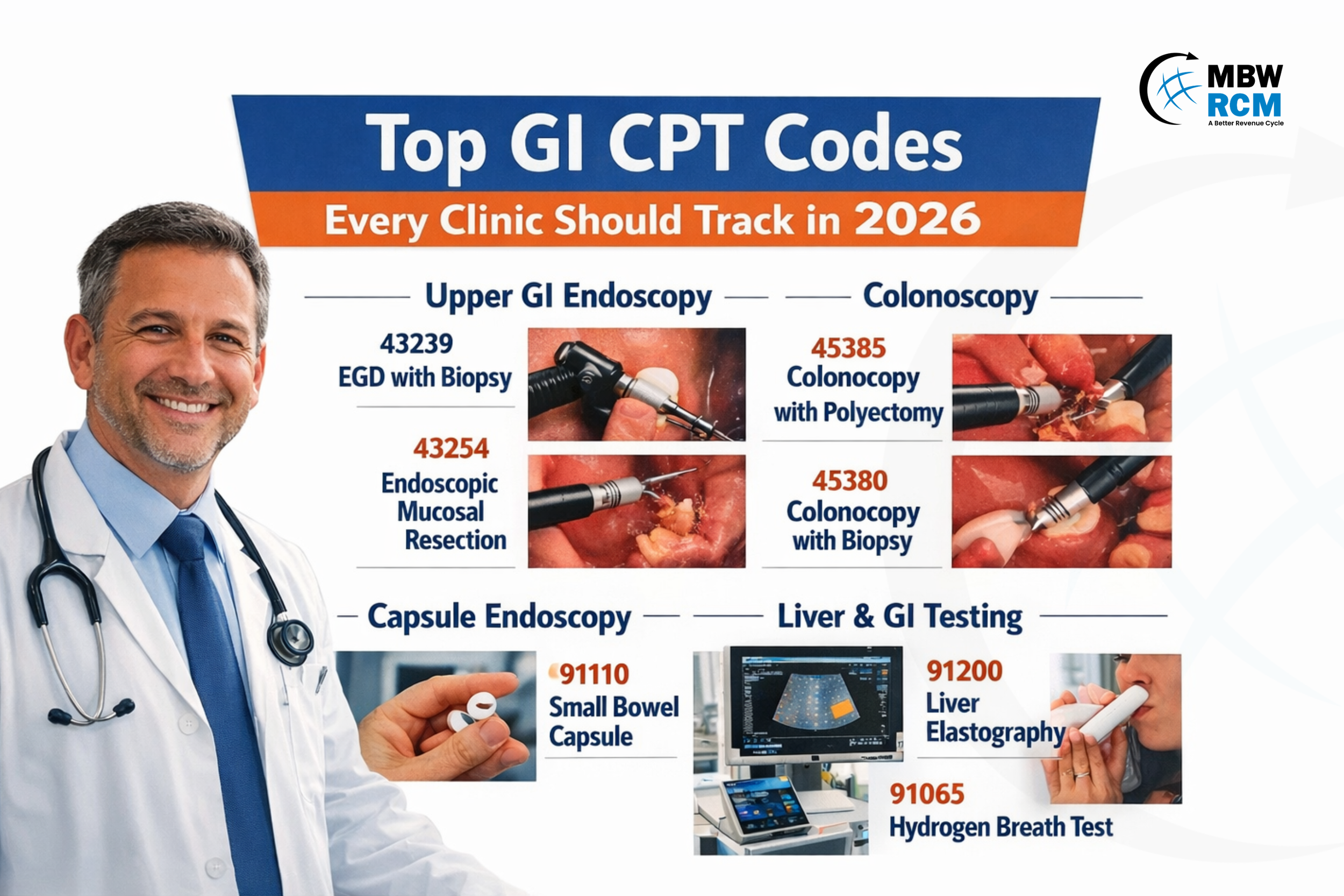
Proper CPT coding is essential for gastroenterology clinics to support compliant clinical documentation and consistent reimbursement as payer requirements and procedure utilization continue to evolve. This blog outlines the Top CPT Codes for Gastroenterology that every Clinic Should Know in 2026, highlighting key procedures and documentation considerations to help improve coding performance and minimize denials.
Table of Contents
1–5: Upper GI Endoscopy (EGD) CPT Codes
Upper GI endoscopy CPT codes are a major contributor to procedural revenue in gastroenterology clinics. These procedures help evaluate mucosal disease, structural abnormalities, bleeding sources, and early malignancy.
From a billing perspective, correctly distinguishing between diagnostic vs therapeutic EGD is important because it directly impacts reimbursement and payer review risk.
1. 43235 — Diagnostic EGD
Commonly performed for:
GERD evaluation
Upper abdominal pain
Iron deficiency anemia workup
Dysphagia screening
Chronic nausea or vomiting
This procedure typically involves systematic mucosal inspection from the upper esophageal sphincter through the second portion of the duodenum. Retroflexion in the stomach is often performed to evaluate the cardia and fundus for hiatal hernia, varices, or proximal gastric lesions.
Documentation Tips
Extent of exam (duodenum reached)
Key findings (esophagitis, gastritis, ulcers, Barrett’s suspicion)
Photo documentation of landmarks
Common Risk
If biopsy is performed but not documented clearly, claims may be downcoded.
2. 43239 — EGD with Biopsy
Why It’s High Volume
Biopsies are frequently performed for:
H. pylori testing
Celiac disease diagnosis
Barrett’s surveillance
Eosinophilic esophagitis evaluation
Biopsies are typically obtained using cold forceps and may involve multiple anatomical sites such as the gastric antrum, gastric body, duodenal bulb, or distal and proximal esophagus depending on the suspected pathology and surveillance protocols.
Documentation Best Practice
Include:
Biopsy location
Number of specimens
Clinical reason for biopsy
Payer Focus Area
Frequent biopsy use can trigger utilization review if indications are unclear.
3. 43251 — EGD with Snare Lesion Removal
Used to remove:
Gastric polyps
Duodenal adenomas
Small mucosal lesions
Lesions are typically resected using electrocautery-assisted hot snare or cold snare techniques depending on lesion size, vascularity, and bleeding risk. Retrieval of the specimen is necessary for histopathological evaluation and confirmation of complete removal.
Documentation Must Include
Lesion size
Location
Resection completeness
Retrieval confirmation
4. 43254 — EGD with Endoscopic Mucosal Resection (EMR)
Used for removal of early-stage mucosal neoplasia and dysplasia.
The procedure generally includes submucosal lifting using saline or viscous lifting agents, followed by cap-assisted or band ligation-assisted resection. Hemostasis may require coagulation, clip placement, or injection therapy depending on bleeding risk.
Documentation Tips
Lesion size and location
Resection technique
Margin status if known
Operational Note
EMR procedures require longer procedure time and higher device cost. Want to know about Gastroenterology EMR Integration and how it supports documentation completeness and billing efficiency?
5. 43266 — EGD with Stent Placement
Performed for:
Malignant esophageal obstruction
Refractory benign strictures
Leak or fistula management
Stent placement usually involves guidewire cannulation of the stricture followed by deployment of a self-expanding metal stent under direct endoscopic visualization, and sometimes fluoroscopic guidance to confirm positioning and luminal patency.
Documentation Must Include
Stricture location and length
Stent type and size
Placement confirmation
Payer Note
Often requires prior authorization and strong clinical justification.
6–10: Colonoscopy CPT Codes
Colonoscopy procedures represent the largest volume and revenue segment under CPT Codes for Gastroenterology, driven by colorectal cancer (CRC) screening, surveillance colonoscopy, and therapeutic polyp removal.
Proper selection and documentation of CPT Codes for Colonoscopy directly impact reimbursement and medical necessity validation. In most GI practices, colonoscopy services make up a significant share of procedural claims, making documentation accuracy essential for strong revenue cycle performance.
6. 45378 — Diagnostic Colonoscopy
Diagnostic colonoscopy is a lower GI endoscopic procedure used for colon evaluation and colorectal cancer screening, often performed before biopsy or polyp removal.
Base procedure used for:
Screening colonoscopy (average or high risk)
Evaluation of GI bleeding
Chronic diarrhea workup
Iron deficiency anemia evaluation
Inflammatory bowel disease assessment
During the procedure, the colonoscope is advanced to the cecum with confirmation of anatomical landmarks such as the appendiceal orifice and ileocecal valve. Careful mucosal inspection during withdrawal is essential for adenoma detection and quality metric reporting.
Documentation Tips
Cecal intubation confirmation
Bowel prep quality (BBPS or equivalent scale)
Withdrawal time documentation
Screening vs diagnostic indication
This is one of the most frequently reported procedures in digestive endoscopy billing and GI procedure coding workflows.
7. 45380 — Colonoscopy with Biopsy
Frequently performed when abnormal mucosa is identified during screening or diagnostic colonoscopy, including suspected colitis, microscopic colitis, or inflammatory bowel disease surveillance.
Biopsies are commonly obtained using cold forceps from multiple colonic segments depending on suspected pathology, especially in chronic diarrhea evaluation or IBD monitoring protocols.
Documentation Best Practice
Biopsy site location
Number of specimens
Indication linked to pathology
Revenue Note
Incorrect screening modifier usage is a common denial reason across CPT Codes for Colonoscopy claims.
8. 45385 — Colonoscopy with Snare Polypectomy
One of the highest value and most utilized procedures in digestive endoscopy services due to colorectal cancer prevention programs and adenoma removal guidelines.
Polyps are typically removed using hot snare electrocautery or cold snare technique depending on polyp size, morphology, and bleeding risk. Larger sessile polyps may require piecemeal resection.
Documentation Must Include
• Polyp size (mm or cm)
• Morphology (pedunculated, sessile, flat)
• Location by colon segment
• Retrieval confirmation
Proper reporting of this procedure is essential for accurate lower GI procedure reimbursement and quality reporting metrics such as adenoma detection rate (ADR).
9. 45390 — Colonoscopy with EMR
Used for removal of large sessile or laterally spreading lesions that cannot be removed via standard snare technique.
The procedure generally includes submucosal lifting injection followed by snare resection. Hemostasis methods such as clip placement or coagulation may be required depending on lesion vascularity and resection size.
Documentation Tips
Lesion size and classification
Injection agent used
Resection technique (en bloc vs piecemeal)
Hemostasis method
Among advanced therapeutic colonoscopy procedures, this service requires strong documentation to support medical necessity during digestive endoscopy billing and GI procedure coding audits.
10. 45381 — Colonoscopy with Submucosal Injection
Submucosal injection is used to improve lesion visualization, create lift before resection, or assist with surgical localization, helping improve safety and resection accuracy during therapeutic colonoscopy.
Commonly used for:
Lesion marking prior to surgical resection
Submucosal lift before EMR or polypectomy
Tattoo placement for future localization
Injection agents may include saline, epinephrine mixtures, or commercial lifting agents depending on procedural goals.
Documentation Must Include
Injection purpose (tattoo vs lift)
Injection location
Agent used if relevant
This code is often underreported in lower GI endoscopy coding but can significantly improve procedure-level revenue capture within digestive endoscopy and GI procedure billing workflows.
11–12: Capsule Endoscopy & Advanced GI Imaging
Capsule endoscopy is an important component within CPT Codes for Gastroenterology, especially for evaluating small bowel pathology when standard endoscopy is inconclusive.
As part of CPT Codes for Endoscopy Procedures, capsule studies support non-invasive mucosal visualization and may contribute to faster diagnosis and Gastroenterology A/R Reduction through earlier treatment planning.
11. 91110 — Capsule Endoscopy (Small Bowel)
Used for evaluation of:
Obscure GI bleeding
Suspected or known Crohn’s disease
Unexplained iron deficiency anemia
The procedure involves ingestion of a wireless capsule that captures images throughout the small intestine and is typically performed after negative EGD and colonoscopy. Interpretation focuses on identifying vascular lesions, ulcers, inflammation, or tumors.
12. 91113 — Capsule Endoscopy (Colon)
Used for patients unable to undergo traditional colonoscopy due to sedation risk, incomplete procedure, or refusal.
Colon capsule studies require strict bowel preparation to ensure adequate mucosal visualization and are used for non-invasive colorectal evaluation in select patients.
13–16: Liver & GI Physiology Testing CPT Codes
Liver and GI physiology testing procedures support functional and metabolic evaluation when structural endoscopy findings are inconclusive. These diagnostic tests are widely used in chronic liver disease monitoring, functional GI disorder evaluation, and reflux disease management. They also support efficient revenue cycle workflows, including Gastroenterology denial management.
13. 91200 — Liver Elastography (FibroScan)
Used for non-invasive assessment of liver fibrosis & steatosis, especially in patients with NAFLD, NASH, hepatitis B, or hepatitis C.
The test measures liver stiffness using transient elastography technology, helping providers stage fibrosis and monitor disease progression without liver biopsy.
14. 91065 — Hydrogen/Methane Breath Test
Used for diagnosis of:
Small intestinal bacterial overgrowth (SIBO)
Lactose intolerance
Fructose malabsorption
The test measures exhaled hydrogen and methane levels after ingestion of specific substrates to evaluate bacterial fermentation patterns.
15. 91010 — Esophageal Motility Study
Used to evaluate esophageal peristalsis and lower esophageal sphincter (LES) function in patients with dysphagia, achalasia, or suspected motility disorders.
High-resolution manometry systems are commonly used to measure pressure patterns along the esophagus.
16. 91035 — Esophageal pH / Impedance Testing
Used for evaluation of refractory GERD symptoms and non-acid reflux.
The test measures acid exposure time and reflux episode correlation with symptoms, often performed while patients continue or discontinue acid suppression therapy depending on clinical indication.
17–18: Anorectal & Functional GI Testing CPT Codes
Anorectal physiology testing evaluates rectal sensation and sphincter function and is commonly reported under CPT Codes for Gastroenterology, supporting GI motility testing reimbursement.
17. 91122 — Anorectal Manometry
Used for evaluation of:
Chronic constipation
Fecal incontinence
Dyssynergic defecation
The test measures anal sphincter pressure, rectoanal inhibitory reflex, and coordination of pelvic floor muscles during simulated defecation using pressure-sensitive catheters. For updates on evolving GI procedure reporting and upcoming coding changes, refer to new CPT codes for GI services:
18. 91120 — Rectal Sensory Testing
Often performed with anorectal manometry to evaluate rectal sensation thresholds and rectal compliance.
This testing helps identify sensory dysfunction contributing to constipation or incontinence and supports targeted pelvic floor therapy planning.
19–20: Advanced Esophageal Function Testing
Advanced esophageal function testing evaluates esophageal motility and is commonly included under CPT Codes for Gastroenterology, supporting esophageal motility testing documentation compliance.
19. 91037 — Esophageal Function Study with Electrode
Used for detailed evaluation of esophageal motility disorders including ineffective esophageal motility, spastic disorders, and pre-surgical assessment for anti-reflux or achalasia procedures.
The test typically measures pressure activity along the esophagus using catheter-based sensors during controlled swallows.
20. 91038 — Extended Esophageal Function Testing (>1 Hour)
Used in complex motility disorder evaluation when prolonged monitoring is required.
Extended testing helps capture intermittent motility abnormalities and provides more comprehensive pressure pattern analysis for difficult-to-diagnose esophageal conditions.
New & Emerging GI CPT Codes to Watch in 2026
Advancements in therapeutic endoscopy and minimally invasive GI procedures are expanding treatment options and reporting pathways, with growing clinical adoption as technology and payer coverage evolve.
Endoscopic Bariatric Procedures
New reporting options are expanding for procedures like:
43889 — Endoscopic Sleeve Gastroplasty (ESG)
Endoscopic Sleeve Gastroplasty is performed using endoscopic suturing to reduce gastric volume and support weight loss.
Clinics offering bariatric endoscopy should monitor payer coverage, prior authorization requirements, and procedure documentation standards.
Start Optimizing CPT Codes for Gastroenterology Now!
Staying updated with commonly used gastroenterology CPT codes is essential for compliant documentation, optimized reimbursement, and reduced claim denials.
Partner with expert Gastroenterology Medical Billing Services to improve billing efficiency and revenue performance. Schedule a consultation now and contact MBW RCM today to get started
FAQs: Gastroenterology CPT Coding & Procedure Guidelines
Request for Information
Facing gastroenterology coding challenges like CPT selection errors, modifier issues, documentation gaps, or GI claim denials? A coding expert can review your workflows and identify improvement areas.
Fill out the form below to connect with an MBW RCM specialist to discuss GI coding challenges and improve your gastroenterology billing performance for 2026