Improve Patient Registration Efficiency in 6 Steps: A Practical Guide
When it comes to the healthcare revenue cycle, your front desk is your financial engine’s ignition switch. Patient registration may look like an administrative formality, but it sets the tone — and the data quality — for everything that follows. From eligibility checks to claims submission and payment collection, the accuracy of this first step determines whether your revenue cycle runs like a well-oiled machine or gets bogged down in denials, delays, and lost income.
Why this matters:
Up to 35% of claim denials originate from errors made during registration and eligibility verification.
Each denied claim costs $25–$118 in rework, plus delays in cash flow.
Patients now pay more out of pocket than ever before, making upfront communication and payment options critical for collections. To learn practical ways to address these challenges, check out this blog on efficient patient registration and communication
Table of Contents
Managing the Revenue Cycle from Registration to Payment with Key Workflow Tips
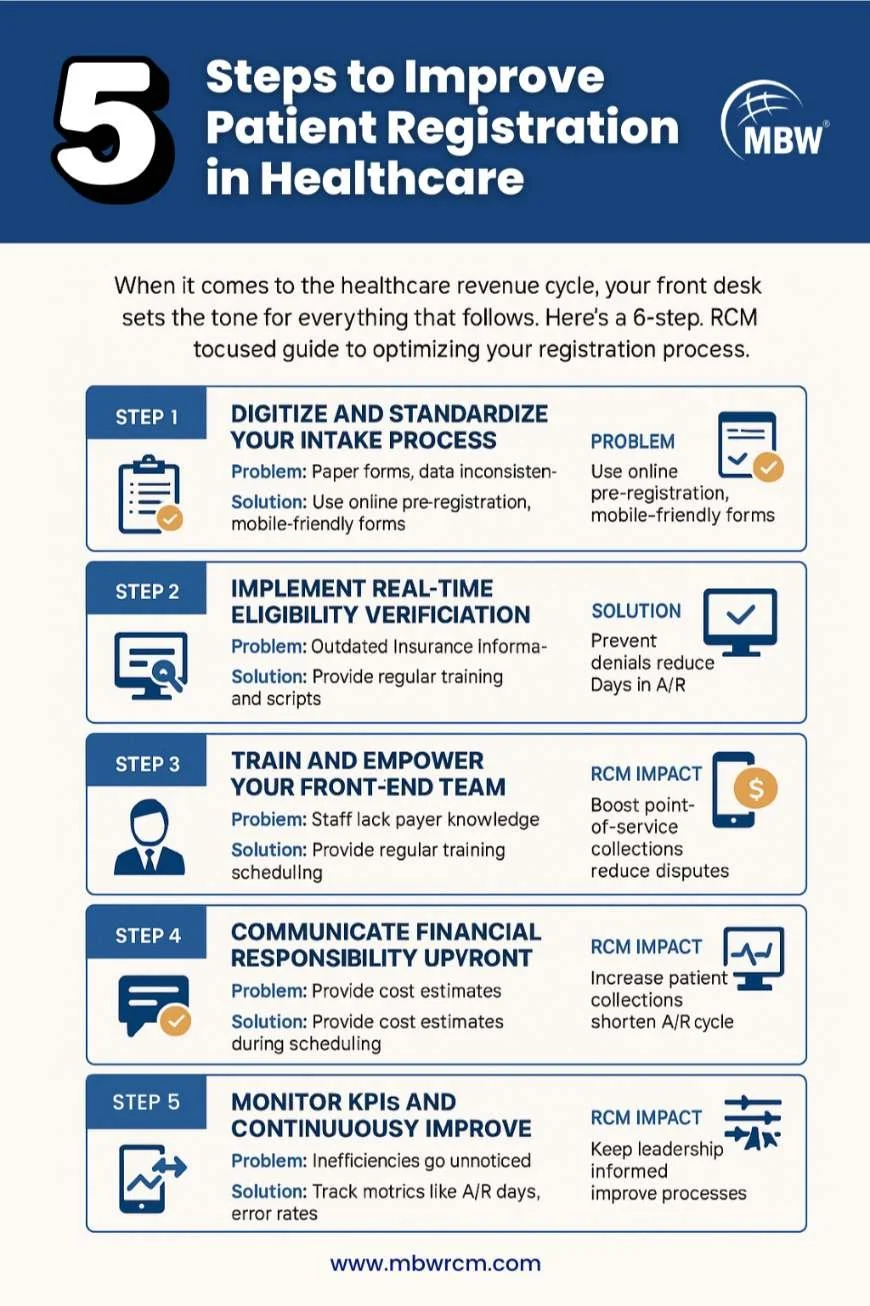
Here’s a 6-step, RCM-focused guide to optimizing your registration process so that your workflow from patient check-in to payment is faster, cleaner, and more profitable.
1. Digitize and Standardize Your Intake Process
The Problem:
Many organizations still rely on paper forms or partially digital systems, creating a hybrid process full of inefficiencies. Patients fill out paper forms in waiting rooms, staff re-enter the data manually, and human error creeps in at multiple points. Handwriting can be illegible, critical fields get skipped, and inconsistencies in date formats or insurance details cause system mismatches.
Real-World Example: A clinic using paper forms had a 7% registration error rate due to transposed digits in policy numbers. This led to dozens of denials monthly, adding thousands of dollars in rework costs.
The Solution:
Digital Pre-Registration: Allow patients to update demographic information, upload insurance cards, and sign consents online before arrival.
Mobile-Responsive Forms: Make sure forms work seamlessly on smartphones — over 70% of patients access portals via mobile.
Standardized Data Fields: Ensure consistent formats for DOB, phone numbers, and insurance IDs across your EHR, practice management, and billing systems.
RCM Impact:
Improves first-pass claim acceptance rates.
Cuts average check-in time by up to 50%.
Ensures all downstream processes work with clean, consistent data.
👉 Check out this resource on improving the patient registration process guide.
2. Implement Real-Time Eligibility Verification
The Problem:
Outdated or incorrect insurance information is a silent revenue killer. Without real-time verification, staff may discover eligibility issues only after the claim is rejected, forcing them to chase corrections and resubmit — sometimes past payer deadlines. Patients often don’t carry updated insurance cards, especially after job changes or plan switches, leading to coverage mismatches.
Industry Context: Over 75% of preventable denials are linked to eligibility and benefit issues, making this one of the most impactful areas to fix.
The Solution:
Use real-time verification tools integrated into your registration software.
Verify coverage, benefits, deductibles, and co-pays before the day of service.
Flag prior authorization requirements immediately to avoid service delays.
RCM Impact:
Prevents denials before claims are submitted.
Reduces Days in Accounts Receivable (A/R) by eliminating back-and-forth with payers.
Improves patient satisfaction by setting accurate payment expectations.
3. Train and Empower Your Front-End Team
The Problem:
Even the best technology is ineffective if staff lack process knowledge or payer-specific expertise. In busy front offices, multitasking under pressure can lead to skipped verification steps or incomplete data capture. Staff turnover worsens the issue, as inexperienced hires may not yet understand the consequences of small mistakes on the RCM pipeline.
Example: One practice found that 60% of its eligibility-related denials came from a single new hire who wasn’t trained on secondary insurance coordination.
The Solution:
Conduct quarterly training on payer policies, documentation standards, and communication best practices.
Use denied claim case studies to turn real-world errors into teachable moments.
Provide standard scripts for collecting sensitive information and explaining costs.
RCM Impact:
Reduces registration error rate to 1–2% industry benchmark.
Builds a patient-first culture that improves satisfaction and retention.
Improves staff efficiency by reducing rework time.
4. Communicate Financial Responsibility Upfront
The Problem:
Patients increasingly expect price transparency — but many practices still avoid cost conversations until after services are rendered. This results in surprise bills, delayed payments, and negative reviews. The lack of upfront communication also means missed opportunities to arrange payment plans or collect deposits before service.
Regulatory Context: CMS Transparency in Coverage and Hospital Price Transparency rules require providers to disclose pricing for common services.
Example: A multi-specialty clinic saw a 25% drop in bad debt after introducing pre-service cost estimates via patient portal messages.
The Solution:
Provide cost estimates during scheduling.
Review them verbally and in writing at check-in.
Use clear, jargon-free language in all financial communications.
RCM Impact:
Boosts point-of-service collections by 20–30%.
Reduces disputed charges and patient complaints.
Improves collection rate by ensuring patients are prepared for their responsibility.
5. Offer Flexible, Digital Payment Options
The Problem:
Relying on paper statements and in-person payments slows cash flow and frustrates patients who expect Amazon-like convenience. In a world where people can pay bills with a few taps on their phone, a lack of mobile or online payment options signals an outdated process — and encourages procrastination in paying balances.
Consumer Insight: 63% of patients say they would switch providers for better digital payment options.
The Solution:
Offer multiple channels: patient portals, mobile apps, text-to-pay, and automated payment plans.
Allow patients to store payment methods securely for recurring charges.
Use automated reminders for upcoming and overdue payments.
RCM Impact:
Increases Patient Responsibility Collection Rate to 90%+.
Shortens A/R cycle.
Reduces reliance on costly collections agencies.
6. Monitor KPIs and Continuously Improve
The Problem:
Without a measurement system, inefficiencies go unnoticed until they become expensive crises. Leadership may assume front-end processes are working smoothly, but without metrics, recurring errors, slow collections, or high A/R days remain hidden.
Example: One hospital reduced its A/R days from 45 to 28 simply by identifying and addressing a recurring insurance verification step that was skipped 12% of the time.
The Solution:
Track these RCM-critical metrics:
Registration Error Rate (Target: 1–2%) — predicts future denials.
Days in A/R (Target: <30 days) — measures overall revenue cycle health.
Patient Responsibility Collection Rate (Target: 90%+) — reflects communication and payment process effectiveness.
RCM Impact:
Keeps leadership informed of bottlenecks.
Supports data-driven process improvements.
Demonstrates ROI of technology and training investments.
For more insights into preventing registration issues and strengthening revenue cycle performance, read our full guide on how to solve patient registration delays.
Integrating These Steps into a Seamless RCM Workflow
When executed together, these steps create a closed-loop workflow:
Pre-visit: Patients complete digital registration and insurance verification occurs automatically.
Check-in: Staff confirm only final details; wait times are minimal.
Service delivery: Providers have accurate insurance and patient data upfront.
Billing: Claims go out clean, without preventable denials.
Collections: Patients receive timely, clear statements with easy digital payment options.
Conclusion
Improving patient registration efficiency is not just operational hygiene — it’s a revenue protection strategy. With a proactive, technology-enabled approach, you can:
Reduce denials before they happen.
Shorten the revenue cycle and accelerate cash flow.
Improve patient trust and satisfaction through transparency and convenience.
Bottom line: If you master the front end, the back end will take care of itself.
Ready to transform your registration process into a profit-driving, patient-pleasing powerhouse?
Our revenue cycle experts at MBW RCM specialize in building front-end workflows that slash denials, accelerate collections, and elevate the patient experience. Let’s talk about how we can optimize your front end — and protect your bottom line. Contact MBW today