Understanding Modifiers in Medical Billing: CPT & HCPCS Level II Modifiers Explained
If you're handling claim submissions, working in a billing office, or trying to reduce denials, this blog is for you. Modifiers in medical billing are short codes that give extra details about a service, like if it was repeated, done on both sides of the body, or done through telehealth.
In this guide, you’ll learn what modifiers are, the different types, when to use them, and how to avoid mistakes—so you can submit claims that are clear, correct, and paid faster.
Understanding Modifiers in Medical Billing
In medical billing, modifiers are two-character codes added to CPT or HCPCS Level II codes to provide extra details about a service or procedure. They do not change the underlying definition of the code but help payers understand why a service was performed in a particular way or under specific circumstances.
For example, if a service requires special handling, a modifier clarifies that information to ensure accurate reimbursement.
Why Are Modifiers in Medical Billing Used?
Modifiers in medical billing are used to tell insurance payers more about the situation. If a service was slightly different or done more than once, modifiers help show that. Without them, claims can be denied or misunderstood. When a procedure requires a modifier, it signals to the payer that the service was distinct or had unique circumstances.
If you're curious about how modifiers work in different medical specialties? Take a look at this blog - ‘’Mastering Modifiers in Podiatry Billing’’
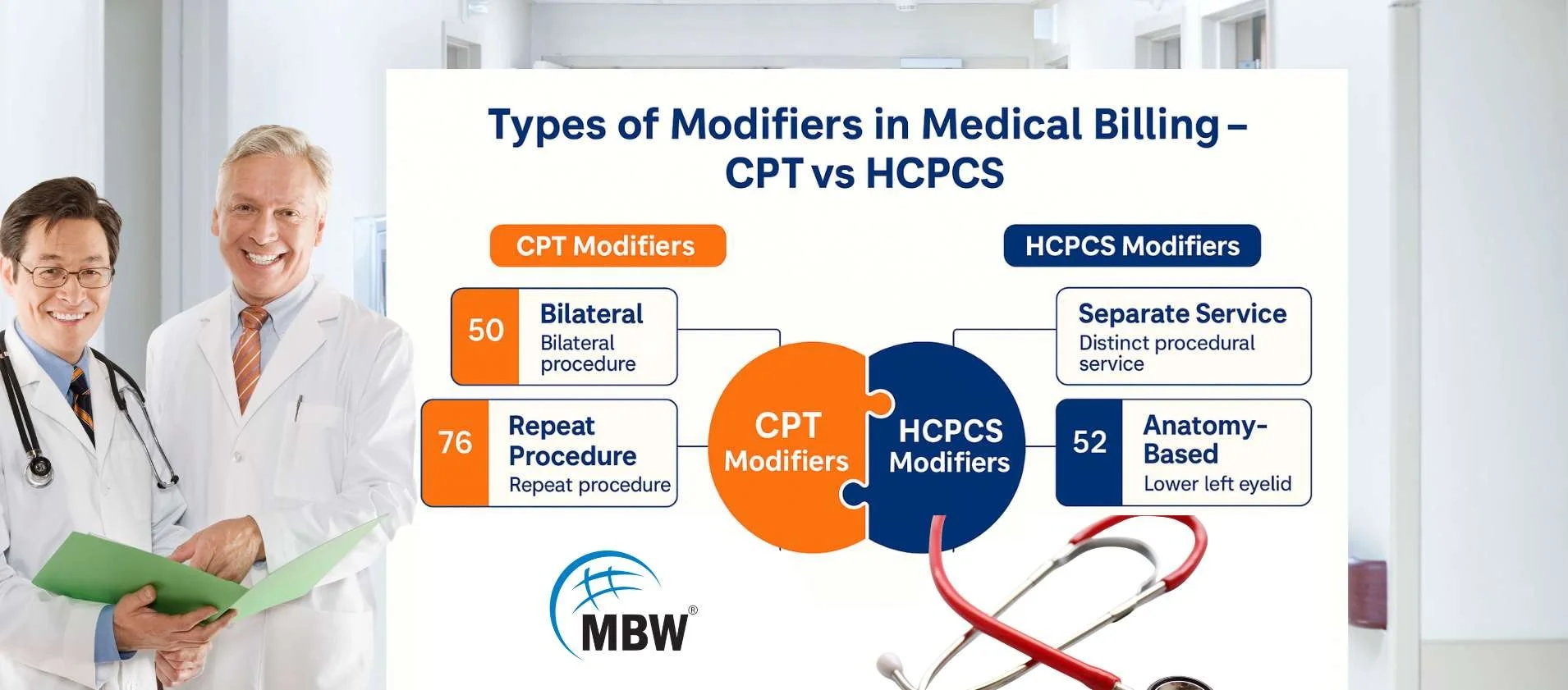
Different Types of Modifiers in Medical Billing
There are two main types of modifiers in medical billing: CPT Modifiers (Level I) and HCPCS Modifiers (Level II). These codes help describe special situations during a medical service, like if the doctor did part of a procedure, did it on one side of the body, or repeated it.
CPT Level I Modifiers
CPT Modifiers are two-digit numeric codes added to standard CPT codes. These are created and maintained by the American Medical Association (AMA). They explain changes such as multiple procedures, incomplete services, or repeated actions during a visit. For example, Modifier 51 shows multiple procedures done during the same session.
These modifiers are most often used for outpatient and physician services. Each CPT modifier helps avoid confusion and supports proper reimbursement by providing extra details.
HCPCS Level II Modifiers
HCPCS Modifiers are two-character alphanumeric codes (a mix of letters and numbers) created by the Centers for Medicare & Medicaid Services (CMS). They are mainly used for Medicare, Medicaid, and other government payers. HCPCS modifiers explain things like the location of service (left or right side), telehealth, ambulance services, or if equipment was rented. To learn more about HCPCS and its role in billing, read our detailed guide on the Healthcare Common Procedure Coding System.
For instance, Modifier RT refers to the right side of the body, and LT refers to the left side. Modifier 95 shows a real-time telehealth service.
These modifiers apply to services or procedures not covered by CPT modifiers, especially for Medicare claims. For example:
Modifier GT: Used for telehealth services provided from a distant site.
Modifier 95: Synchronous telemedicine service rendered via real-time interaction.
Modifier QW: For CLIA-waived tests.
Telehealth Billing and Modifiers
With the growth of telehealth, understanding how to use modifiers in telehealth billing is critical. Medicare, for example, requires specific HCPCS Level II modifiers to indicate whether a telehealth service was provided at a distant site or if certain technology requirements were met.
For Example:
Modifier 95: Ensures telehealth visits are recognized as valid virtual encounters.
Modifier FQ or FR: Used for audio-only or split/shared telehealth services in some cases.
Proper use of telehealth-related modifiers ensures compliance and accurate payment for remote care services.
List of Commonly Used Modifiers in Medical Billing
If you’re new to billing, it’s helpful to know which modifiers are used most often. These commonly used modifiers help explain special situations, like if a service was done on both sides of the body, if more than one procedure was performed during the same visit, or if a service was provided via telehealth. Understanding these modifiers helps reduce claim denials and supports cleaner, faster reimbursement.
Here is a list of some common modifiers in medical billing with what they mean:
| Modifier | Meaning | Example |
|---|---|---|
| 25 | Separate service during same visit | Office visit and minor surgery |
| 26 | Professional component only | Reading an X-ray, not taking it |
| 59 | Different procedure, same session | Two unrelated procedures on same day |
| 50 | Both sides of the body | Surgery on both knees |
| 51 | Multiple procedures | More than one surgery in same session |
| 76 | Repeat procedure by same doctor | Repeat EKG on same day |
| 95 | Telehealth service | Online doctor visit |
| GT | Telehealth via live video | Real-time video consultation |
Examples of Common Modifiers in Medical Billing
Understanding real-life examples makes it easier to know when and how to use modifiers in medical billing. These examples show how modifiers help explain what happened during a patient visit. Without the correct modifier, insurance companies may reject or underpay a claim because they don’t have enough information.
Modifier 25: A patient comes in for a routine check-up and receives a minor surgical service during the same visit. Modifier 25 clarifies that the evaluation and the procedure were separate and both medically necessary.
Modifier 59: A doctor removes a skin lesion and performs a biopsy during the same visit. Since these are distinct procedures, Modifier 59 is used to show they should be billed separately.
Modifier 50: A procedure is done on both sides of the body—for example, injections in both knees. Modifier 50 indicates that the procedure was performed bilaterally.
Modifier 26: A radiologist reads an X-ray taken at another facility. Modifier 26 is applied to indicate that only the professional interpretation was done, not the technical part of the test.
Modifier 95: A mental health session takes place via live video. Modifier 95 marks the visit as a telehealth service delivered in real time.
These examples help clarify when modifiers are necessary to avoid denials and explain services correctly on a claim.
“Modifiers are like GPS—use the wrong one, and your claim ends up lost.”
Quick Reference Table for Modifiers
| Situation | Modifier to Use |
|---|---|
| Procedure repeated same day | 76 |
| Telehealth service | 95 or GT |
| Both limbs involved | 50 |
| More than one procedure in one session | 51 |
| Separate service same day | 25 |
How to Use Modifiers in Medical Billing the Right Way?
To use modifiers correctly, start by checking if the service was unusual, repeated, or done with another procedure. If so, a modifier may be needed. Always include proper documentation like doctor notes to explain why the modifier applies. Also, follow each payer's rules—what works for one insurance may not work for another. Use coding tools to stay current and avoid common billing mistakes.
Know payer rules: Some payers have unique requirements for modifier usage.
Understand when a service requires a modifier: Use it to avoid bundling or claim denials.
Document thoroughly: Proper documentation supports why a modifier was used.
Stay current: Regularly review payer updates, especially for HCPCS Level II codes and telehealth regulations.
Common Mistakes When Using Modifiers
Even experienced billers can make errors with modifiers. Below are the most common mistakes, broken down to help you spot and avoid them in real scenarios:
Using Modifier 59 Instead of X Modifiers
Modifier 59 is often overused. CMS encourages using XE, XP, XS, or XU to give more precise details. Using 59 when another modifier fits better may lead to claim rejections.
Missing Documentation
Every modifier you use must be backed up by records. Without progress notes, operative reports, or written justification, the claim can be denied—even if the modifier is correct.
Applying the Wrong Modifier
Sometimes, a modifier is used just to get a claim paid, not because it’s accurate. This can trigger audits or denials. Always match the modifier to the exact service and situation.
Ignoring Payer-Specific Rules
Each insurance provider may have its own modifier guidelines. What’s allowed by Medicare might not apply to a private payer. Always check payer policies before submission.
Stacking Incompatible Modifiers
Using multiple modifiers on one code without understanding their relationship can confuse the claim system. For example, using Modifier 25 with Modifier 59 without justification may raise red flags.
Avoiding these mistakes helps you submit cleaner claims, get paid on time, and reduce the chances of audits or denials.
“Guessing a modifier? Might as well roll dice on your claim.”
What Are Telehealth Modifiers in Medical Billing?
Telehealth modifiers in medical billing indicate that the service was provided remotely, often via video or audio communication. These codes inform payers that the encounter occurred outside of a traditional office setting while still meeting all applicable coverage and reimbursement criteria.
The two most widely recognized telehealth modifiers are:
Modifier 95: This is used for real-time, synchronous telemedicine visits where the provider and patient interact via live audio-video. It’s commonly accepted by both commercial and government payers post-COVID.
Modifier GT: This also identifies synchronous telehealth services but was primarily used in older billing systems and for certain Medicare plans. Some payers still require GT instead of 95, depending on the contract or billing platform.
Always check payer-specific guidelines, as some insurers may require additional documentation like the place of service code (e.g., POS 02 or 10) to confirm a telehealth setting.
Telehealth modifiers are critical to getting reimbursed correctly for virtual care services, especially in a healthcare landscape where remote care continues to grow.
Understanding Modifier 59 and the X-Series Modifiers (XE, XP, XS, XU)
Modifier 59 is used to show that two procedures done on the same day are separate and need individual reimbursement. To make this clearer and reduce misuse, CMS introduced the X-series modifiers (XE, XP, XS, XU), each giving a specific reason why the service is distinct.
When to Use Modifier 59
Use Modifier 59 only when none of the X-series modifiers apply. It should be a last option to indicate that a procedure is distinct and not part of the other services performed during the same encounter. This might include services that occur at different times or locations but are billed together.
When to Use XE, XP, XS, or XU
The X-series modifiers should be used when they clearly describe why a procedure is separate from others performed on the same day. These modifiers provide more precise context than Modifier 59 and are preferred by CMS to reduce misuse.
XE (Separate Encounter): Use when the procedures occurred during different visits on the same day.
XP (Separate Practitioner): Apply when a different healthcare provider performed the additional service.
XS (Separate Structure): Use when the same service was provided to a different body site or organ system.
XU (Unusual Non-Overlapping Service): Choose when a service is distinct due to unusual circumstances not commonly linked with the main procedure.
Correctly using modifiers in medical billing leads to cleaner claims, faster payments, and reduced denials by clearly explaining the services provided. Whether you’re billing for in-person services, preventive care, or telehealth visits, understanding when a service requires a modifier—and applying the correct CPT or HCPCS Level II modifiers—ensures you get paid accurately while staying compliant.
Need ongoing billing support or looking for reliable RCM solutions? Visit MBW RCM to learn how we can support your workflow. Have questions or want personalized help? Talk to us our billing experts are ready to assist you.