Dermatology Billing Challenges: Expert Solutions for Accurate Coding and Faster Payments
Dermatology practices are committed to improving patients’ skin health—but poor billing and coding can quietly undermine a practice’s financial stability.
Research shows medical providers lose 10% to 30% of potential revenue due to billing inefficiencies, coding mistakes, and delayed or denied claims. Dermatology, with its procedural complexity and cosmetic/medical overlap, is especially vulnerable.
As one clinic manager said, “The billing department is where the money disappears—unless it’s managed with precision.”
In this guide, we break down the biggest challenges in dermatology billing, the costly mistakes to avoid, and the expert-backed strategies that can streamline your revenue cycle, reduce denials, and accelerate payments.
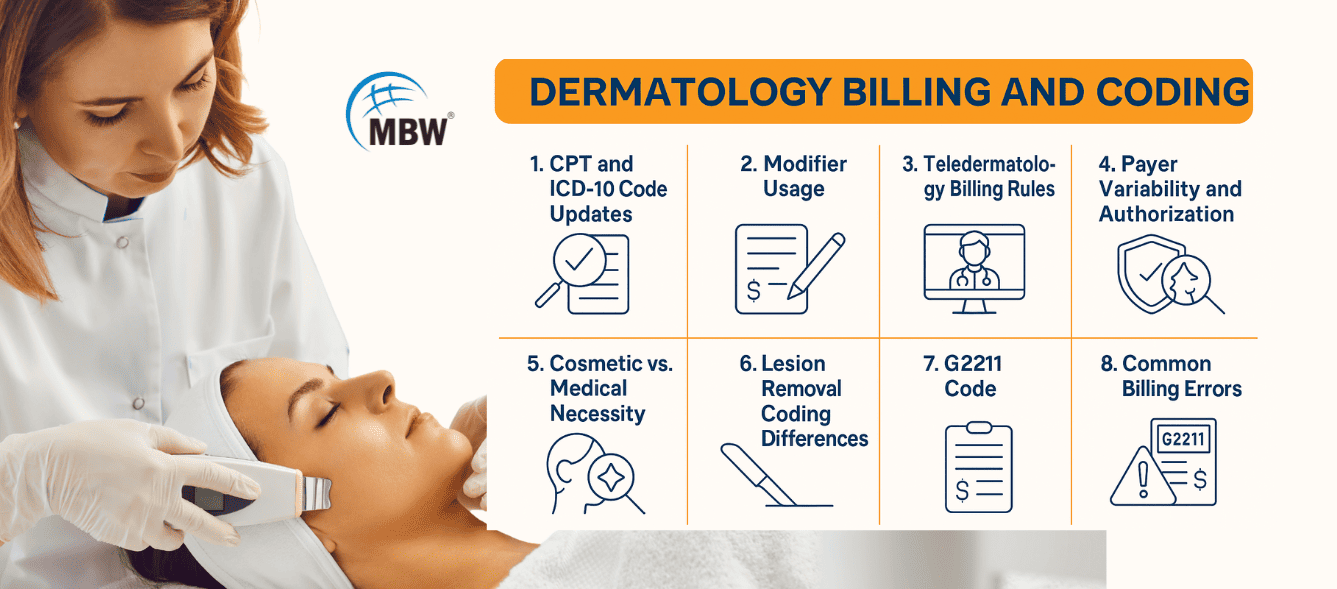
Why Is Dermatology Billing So Complex?
Dermatology billing is not just about entering codes—it requires accuracy, documentation, and knowledge of nuanced rules that change frequently. Here’s why many practices struggle:
1. Constant Changes to CPT and ICD-10 Codes
Dermatology procedures like biopsies, lesion removals, and destructions are regularly updated in CPT® and ICD-10-CM code sets. Using outdated codes can lead to underpayments or outright denials.
Refer to AMA’s CPT® code updates to stay current with annual changes.
2. Modifier Usage Is Under High Scrutiny
Modifiers such as:
25 (significant, separate E/M service)
59 (distinct procedural service)
are essential in dermatology billing—but misused, they’re a red flag for audits or automatic denials.
3. Teledermatology Billing Rules Are Evolving
Many practices embraced teledermatology, but not all have adapted to the changing reimbursement models for virtual visits. Each payer has different requirements for modifiers, documentation, and coverage. Read more about teledermatology billing in 2025
4. Payer Variability and Prior Authorization Requirements
Coverage for dermatology procedures like Mohs surgery or Botox for hyperhidrosis varies between payers. Failing to verify eligibility or obtain prior authorization causes preventable delays and denials.
5. Distinguishing Cosmetic from Medically Necessary Procedures
Many dermatologic services can be perceived as cosmetic. Without supporting documentation—including diagnosis codes, symptoms, and clinical photos—insurers are likely to deny coverage.
6. Lesion Removal Coding Depends on Intent and Technique
Is it a biopsy, a shave removal, or an excision? The answer depends on what was intended, how deep the procedure went, and often, the pathology report. Coding errors in this area are common and costly.
7. G2211 Code: Small Detail, Big Impact
The Medicare add-on code G2211 is designed for complex patient relationships, but it comes with limitations. You cannot bill it with certain procedures or when using modifier 25. Misapplication leads to denials.
The 7 Most Costly Dermatology Billing and Coding Mistakes
Many billing issues are preventable. Below are the most common errors that reduce revenue—and how to address them.
1. Incomplete Clinical Documentation
If it's not properly documented, it can’t be billed. Missing lesion sizes, unclear procedures, or vague diagnoses often lead to denials or underpayment.
2. Outdated or Incorrect Coding
Using outdated CPT or ICD-10 codes, or billing incorrectly for the services provided, causes denials and leaves revenue on the table.
3. Modifier Errors
Modifiers are necessary, but even minor misuse—especially of 25, 59, or 51—can result in denials or compliance flags.
4. Unbundling of Services
Unbundling—billing separately for services that should be coded together—is a common mistake that can trigger audits and repayment demands.
5. Lack of Eligibility Verification and Authorization
Without prior authorization or eligibility checks, claims are likely to be rejected. Up to 70% of denied claims could have been prevented with proactive verification.
6. Failure to Follow Up on Denials
Many denied claims are recoverable, yet go unaddressed. Experts estimate 60–90% of denials can be overturned with timely appeals and corrected submissions.
7. Poor Patient Communication on Billing
Patients who don’t understand their insurance coverage or payment responsibilities are less likely to pay on time. Clear, upfront communication is essential.
5 Expert Strategies to Improve Dermatology Billing Performance
Addressing billing challenges doesn’t just improve revenue—it also improves compliance, staff efficiency, and patient satisfaction. Here’s how to get started:
1. Improve Documentation Standards
Include precise diagnosis, treatment rationale, and lesion measurements
Use clinical photos for procedures that may be questioned as cosmetic
Ensure each procedure code is supported by a specific and relevant ICD-10-CM code
2. Provide Ongoing Training for Billing and Clinical Staff
Train regularly on annual CPT, ICD-10, and HCPCS code changes
Offer specialized training on commonly misused modifiers
Clarify the procedural differences between biopsies, excisions, and lesion destruction techniques
3. Automate and Integrate with the Right Technology
Use an integrated EHR and billing platform to reduce manual entry errors
Implement claim-scrubbing tools to catch issues pre-submission
Automate eligibility checks and prior authorization workflows
Use analytics tools to track key performance indicators like denial rates and AR days
4. Strengthen Revenue Cycle Management (RCM) Workflows
Verify insurance and secure prior authorizations before appointments
Submit clean claims quickly—within 24–48 hours post-visit
Follow up consistently on all denials with appeals and resubmissions
Offer transparent billing communication and flexible payment options for patients
5. Consider Outsourcing Dermatology Billing
If internal billing challenges persist, outsourcing to a professional billing partner can:
Reduce administrative burden
Improve coding accuracy and compliance
Accelerate cash flow
Increase collection rates
Look for billing companies with dermatology-specific experience to ensure the best results.
Final Thoughts: Your Path to Financial Stability Starts with Better Billing
Dermatology billing is complex—but manageable with the right systems, training, and technology in place. By focusing on documentation accuracy, modifier compliance, real-time eligibility checks, and claim follow-up, practices can recover lost revenue and strengthen their financial position.
And when internal resources are stretched, outsourcing to a specialized billing partner may be the best investment you can make.
“The best way to cure a billing headache is to prevent it in the first place.”
Looking for Dermatology Billing Expertise?
We specialize in dermatology revenue cycle management, coding compliance, and denial resolution. Contact us today to learn how we can help your practice streamline billing, reduce denials, and improve cash flow—so you can stay focused on patient care.