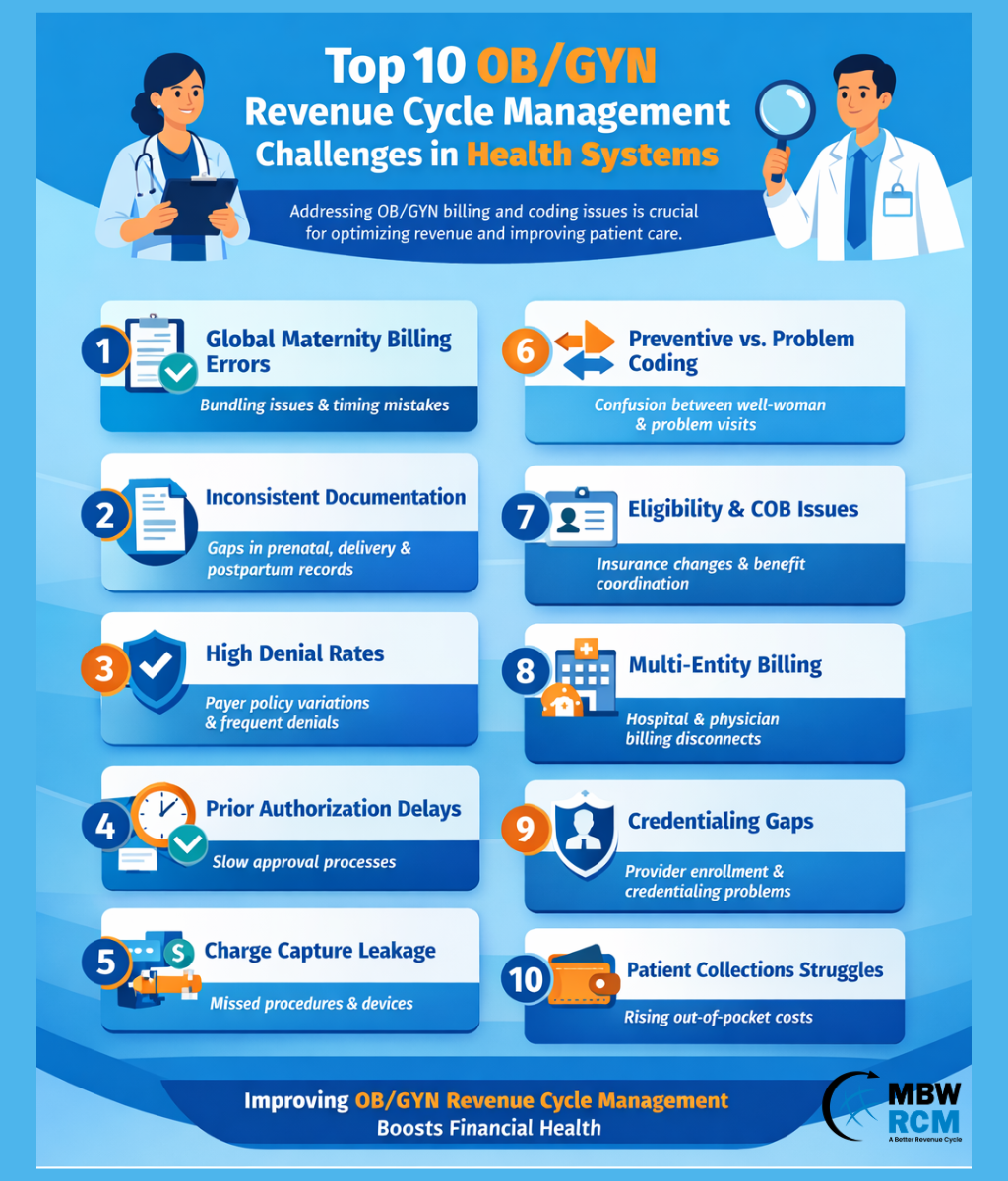
Top 10 OB/GYN Revenue Cycle Management Challenges in Healthcare
OB/GYN Revenue Cycle Management is one of the most complex and high-risk revenue functions within a health system. Unlike specialties driven by isolated encounters, OB/GYN care spans preventive services, chronic condition management, in-office procedures, surgical interventions, and long-duration maternity episodes.
Each phase of care introduces different documentation, coding, billing, and reimbursement requirements—often governed by payer-specific rules that change frequently.
Because OB/GYN Revenue Cycle Management is episode-based rather than visit-based, even minor operational gaps can create downstream financial consequences. A missed eligibility update in the first trimester, an undocumented complication during delivery, or an authorization lapse for imaging can lead to denials months later.
Understanding how these breakdowns occur is essential for strengthening women’s health RCM performance. This in-depth overview of OB/GYN medical billing fundamentals provides helpful background for navigating these complexities.
Below are the most pressing OB/GYN Revenue Cycle Management challenges facing health systems today—and actionable strategies to resolve them.
Table of Contents
1) Global maternity billing complexity and timing errors
Global maternity billing is the single most defining feature—and risk factor—of OB/GYN Revenue Cycle Management. Because prenatal care, delivery, and postpartum services are bundled into a global obstetric package, accurate reimbursement depends on treating maternity as a continuous episode of care rather than a series of discrete visits.
In health systems, maternity care often spans multiple practices, providers, and facilities. Without unified episode tracking, billing teams may struggle to determine when global billing applies, when services should be unbundled, or how to handle transfers of care.
Why it happens
Global maternity billing errors occur when pregnancy episodes are not clearly initiated, tracked, and closed. Patients may change providers mid-pregnancy, deliver at a different hospital, or experience complications that alter billing rules. Documentation of exceptions—such as high-risk conditions or additional procedures—is often inconsistent, leaving billing teams without the clarity needed to code accurately.
RCM impact
In OB/GYN Revenue Cycle Management, global billing errors can result in significant underbilling or overbilling. Health systems may miss entire global claims, trigger payer audits, experience delayed reimbursement, or face recoupments months after payment. These issues directly impact cash flow, compliance risk, and revenue predictability.
Fixes that work
Implement episode-based maternity tracking across all care settings
Standardize global billing rules and exception handling
Align clinical documentation with billing milestones
Many organizations rely on specialized OB/GYN billing and coding services focused on maternity revenue integrity to reduce risk in this high-dollar area.
2) Inconsistent documentation across prenatal, delivery, and postpartum care
Documentation is the backbone of OB/GYN Revenue Cycle Management, yet it is frequently fragmented across outpatient clinics, labor and delivery units, and postpartum care settings. This fragmentation undermines coding accuracy and weakens medical necessity support.
Why it happens
Different providers document care at different stages using varying templates and standards. Prenatal risk factors may not flow into delivery documentation, and postpartum visits may be delayed, virtual, or missed altogether. This lack of continuity is common in women’s health RCM environments.
RCM impact
Incomplete or inconsistent documentation leads to downcoded claims, missed complication capture, and increased denials. In OB/GYN medical billing, missing risk factors can also reduce reimbursement for high-acuity cases and weaken appeal success.
Fixes that work
Standardize OB/GYN documentation templates system-wide
Conduct concurrent documentation audits during pregnancy
Enforce structured postpartum visit documentation
3) High denial rates due to payer policy variation
Denials are a persistent challenge in OB/GYN Revenue Cycle Management, largely because payer coverage rules vary widely for women’s health services. Ultrasounds, genetic testing, infertility-related procedures, and surgical interventions are especially vulnerable.
Why it happens
Providers often order services based on clinical guidelines, but payer policies may impose stricter requirements. When documentation does not explicitly align with payer language, claims are denied for lack of medical necessity—even when care was appropriate.
RCM impact
Denials increase accounts receivable days, drive up administrative costs, and delay revenue recognition. In high-volume OB/GYN departments, unmanaged denial trends can erode margins quickly.
Fixes that work
Maintain payer-specific OB/GYN policy libraries
Align order sets with coverage requirements
Track denial trends by service and payer
Health systems often adopt advanced OB/GYN denial management strategies proven to reduce payer pushback to stabilize reimbursement.
4) Prior authorization delays and breakdowns
Prior authorization is now a central pressure point in OB/GYN Revenue Cycle Management. Imaging, procedures, and specialty medications increasingly require approval, and failures in this process often surface only after services are rendered.
Why it happens
Authorization workflows are frequently decentralized, manually tracked, and disconnected from scheduling systems. Staff turnover and payer variability further complicate compliance.
RCM impact
Authorization failures lead to avoidable denials, rescheduled services, and patient dissatisfaction. Over time, they also increase administrative burden and slow revenue cycles.
Fixes that work
Centralize OB/GYN prior authorization teams
Track authorization status in real time
Link scheduling to authorization readiness
5) Charge capture leakage for procedures and devices
Accurate charge capture is critical in OB/GYN Revenue Cycle Management due to the high volume of in-office procedures and billable supplies.
Why it happens
Charges may be missed when documentation, inventory, and billing workflows are not aligned. Devices such as IUDs and implants are especially vulnerable to leakage.
RCM impact
Missed charges quietly erode revenue and distort financial reporting, making it difficult to assess true women’s health service line performance.
Fixes that work
Audit high-volume OB/GYN procedures
Reconcile device inventory to claims
Embed charge prompts into clinical workflows
6) Preventive vs. problem visit coding confusion
Preventive care is foundational to women’s health, but it is also a frequent source of coding errors in OB/GYN Revenue Cycle Management.
Why it happens
Providers address both preventive and problem-focused concerns in a single visit, but documentation may not clearly support separate billing.
RCM impact
Under-coding reduces revenue, while over-coding increases audit and refund risk. Patient confusion over unexpected bills also rises.
Fixes that work
Educate providers on separate E/M documentation
Set expectations with patients upfront
Improve transparency in visit summaries
7) Eligibility and coordination of benefits (COB) challenges
Eligibility management is uniquely complex in OB/GYN Revenue Cycle Management because pregnancy often coincides with insurance changes.
Why it happens
Patients may change employers, plans, or Medicaid eligibility mid-pregnancy, and newborn enrollment adds further complexity.
RCM impact
Eligibility errors lead to denials, rework, and delayed reimbursement—often months after services were rendered.
Fixes that work
Re-verify coverage at pregnancy milestones
Address COB issues proactively
Educate patients on reporting changes
8) Multi-entity billing across hospital and physician services
OB/GYN episodes often generate multiple claims across billing entities, increasing coordination challenges.
Why it happens
Physician, hospital, anesthesia, lab, and imaging billing functions often operate independently.
RCM impact
Misaligned claims increase denials, AR days, and patient confusion.
Fixes that work
Align diagnosis coding across entities
Coordinate billing timelines
Improve patient communication
9) Credentialing and enrollment gaps
Provider enrollment issues pose immediate risk in OB/GYN Revenue Cycle Management, especially with rotating staff models.
Why it happens
Credentialing and scheduling workflows are not tightly integrated.
RCM impact
Claims billed under non-enrolled providers result in hard denials and lost revenue.
Fixes that work
Track enrollment status centrally
Block scheduling for non-enrolled payers
Standardize onboarding processes
10) Weak patient collections amid rising out-of-pocket costs
Patient responsibility continues to rise, placing pressure on OB/GYN Revenue Cycle Management teams to improve collections without harming patient trust.
Why it happens
Estimates are inaccurate, payment options are limited, and financial conversations occur too late.
RCM impact
Bad debt increases and patient satisfaction declines.
Fixes that work
Provide early, accurate estimates
Offer flexible payment plans
Train staff in empathetic counseling
Health systems often benchmark against top-performing OB/GYN billing companies known for revenue and patient experience excellence to guide improvement efforts.
Final takeaway
OB/GYN Revenue Cycle Management demands an episode-based, specialty-specific approach. Health systems that invest in women’s health RCM expertise, denial prevention, and patient-centered financial workflows are far better positioned to protect margins while supporting high-quality care.
FAQs: OB/GYN Revenue Cycle Management Challenges
Request for Information
Struggling with OB/GYN Revenue Cycle Management issues like maternity billing errors, denials, or workflow inefficiencies? Complete the form below to request a complimentary OB/GYN revenue cycle review. Our experts will identify revenue gaps, reduce denials, and help optimize your OB/GYN billing performance.