Top 10 Qualities of Radiology Billing Experts
A Radiology billing experts supports imaging centers and hospitals in managing claims, coding, and payer rules. After all, radiology billing is unlike other specialties. Accordingly, in this guide, we highlight the 10 most important qualities found in leading U.S. radiology billing companies, so you can compare providers with confidence.
The U.S. imaging services market was valued at USD 156.1 billion in 2025, with projected growth at ~4.3% CAGR through 2030. At the same time, denial rates are rising, with initial claim denials reported at nearly 12% in 2024 and continuing upward into 2025. This makes it clear: your billing partner should do more than just get by — they should help your team succeed.
Table of Contents
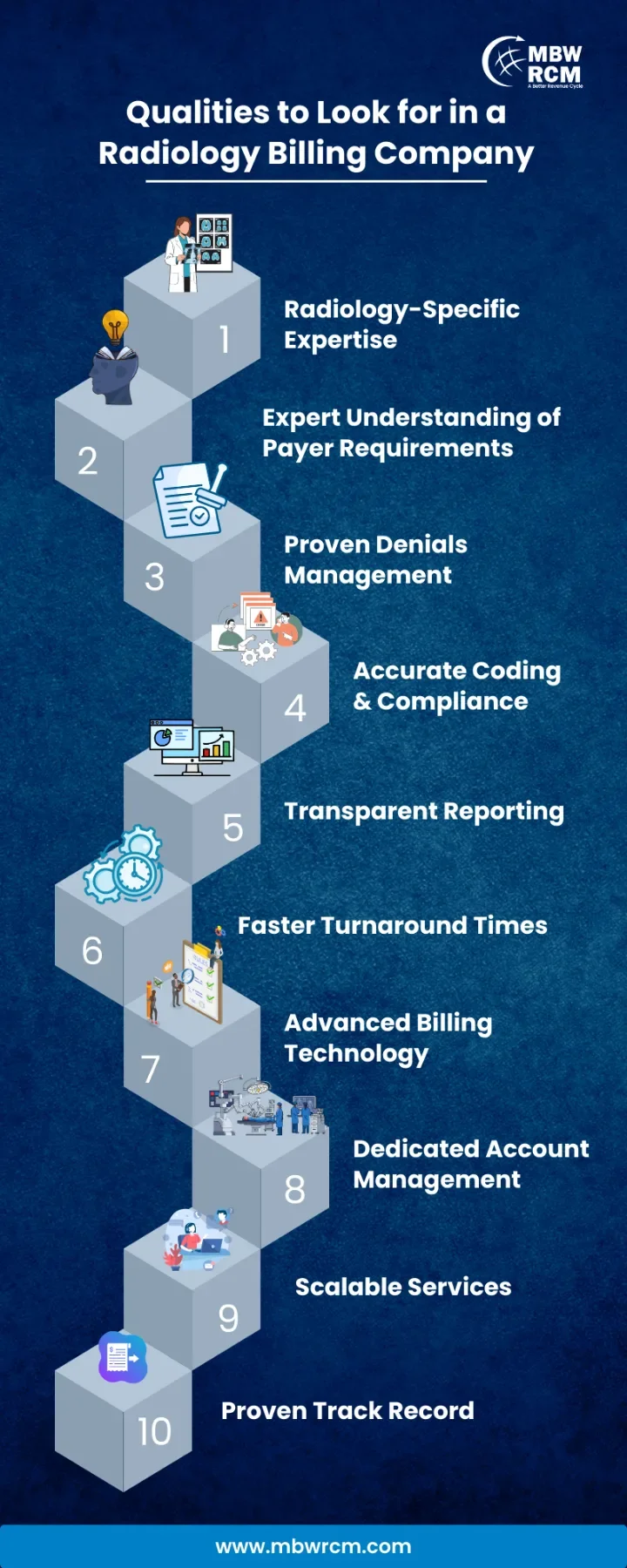
Here Are the Top Qualities of a Radiology Billing Experts
Radiology billing comes with unique codes, modifiers, and payer rules that differ from other specialties. A reliable partner reduces errors, limits denials, and strengthens reimbursements. Below are the 10 key qualities to look for when choosing a radiology billing experts.
1. Radiology Domain Expertise & Niche Focus
A radiology billing experts must specialize in imaging, not general medical billing. When a partner knows CPT codes specific to CT, MRI, nuclear medicine, and interventional radiology, they reduce errors. For instance, applying modifier 26 vs TC properly.
This depth minimizes denials for radiology claims and stays current with changes in imaging reimbursement.
2. Certified Coders Skilled in PC/TC & Modifiers
Certified coders who master component splits and modifiers yield better claim outcomes. Given the complexity of radiology coding (e.g., distinguishing professional vs technical component billing), only coders well versed in those rules can reduce denials. Incorrect modifier use is a top cause of claim rejection, which is why relying on trusted radiology coding guidelines is critical for compliance and reimbursement accuracy.
3. Proactive Denial Prevention & Management
Because denial rates in radiology can reach double digits, a billing partner must prevent denials, not just manage them reactively. Effective partners use pre-submission checks, trend analytics, root cause tracking, and timely appeals.
Denial Prevention Focus Areas:
4. Compliance & HIPAA / Audit Readiness
Because imaging claims often involve high cost and scrutiny, compliance is non-negotiable. Qualified radiology billing experts must enforce HIPAA, stay aligned with payer rules, audit internally, and maintain documentation. Incorrect modifier use or lack of medical necessity proof is a frequent reason for denial. For official policy standards on radiology services, see the CMS Radiology Billing Manual.
5. Technology Integration with RIS / PACS / EHR
A billing partner must integrate cleanly with your imaging systems. When data flows from RIS/PACS/EHR directly into billing platforms, manual errors drop and processing speeds rise.
Tech Capabilities to Check:
6. Transparent Reporting & KPI Dashboards
You should see your metrics — not wait for static PDFs. Experienced radiology billing experts provide dynamic dashboards with KPIs like clean claim rate, net collection rate, days in A/R, and denial breakdowns. Providers who follow best practices in radiology billing and coding consistently outperform other practices in reporting transparency and claim cycle efficiency.
7. Clear & Comprehensible Pricing
Pricing transparency is critical when selecting radiology billing experts. Some partners charge a percentage of collections, while others use a flat per-claim fee. The agreement should clearly state which services are included, such as coding audits, credentialing, and analytics. Without this clarity, unexpected add-on charges can erode trust and inflate costs.
“Confusing fees are like dark tunnels — the further you walk, the less light you see.”
8. Strong Reputation & Client References
Qualified radiology billing experts should be able to share client case studies, especially in imaging practices, and your evaluation include speaking with references. Look for positive outcomes, longevity, and communication ease. To see how industry standards are defined, the Society of Interventional Radiology’s coding and reimbursement guidelines provide useful benchmarks that reflect what top-performing practices follow.
9. Scalability & Flexibility
As imaging volume rises or new modalities get added, your billing partner must scale too. Whether it’s adding coder capacity, handling new site workflows, or shifting between CT, PET, MRI — adaptability matters.
10. Continuous Education & Coding Updates
Codes, payer rules, and imaging technology evolve. The right billing company invests in ongoing training for coders, monitors CMS/AMA/Payer bulletins, and updates processes accordingly. The HCFA 1500 form used by radiologists is an important reference for maintaining claim compliance and reimbursement accuracy.
Radiology practices deal with coding challenges, denials, and payer rules every day. The right radiology billing experts provides solutions through expertise, compliance, clear reporting, and scalable support. With the right partner, your team can reduce errors, improve reimbursement, and stay focused on patient care.
For specialized radiology billing services, Contact MBW RCM today and let our experts provide the solutions your practice needs.
FAQs on Radiology Billing Experts & Imaging Revenue Cycle Management
Request for Information
Is your radiology practice facing challenges with coding errors or denied claims? Partnering with the right billing experts can optimize workflows and keep reimbursements consistent. Fill out the form below to see how MBW RCM can strengthen your revenue cycle.