Catheter-Associated Urinary Tract Infections: From Diagnosis to ICD-10-CM Coding
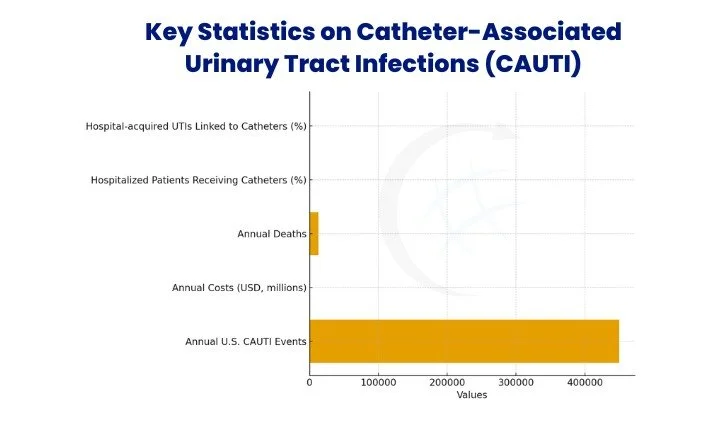
Catheter associated urinary tract infections (CAUTIs) remain among the most frequent healthcare-associated infections, affecting hospital and long-term care settings alike. In fact, each year in the U.S., there are an estimated ~450,000 CAUTI events, accounting for $450 million+ in healthcare costs and about 13,000 deaths. Precise diagnosis, strong prevention, and correct ICD-10-CM coding thus matter deeply to both patient safety and institutional accountability.
Table of Contents
Defining Catheter-Associated Urinary Tract Infections (CAUTI)
A catheter-associated urinary tract infection (CAUTI) develops when bacteria or fungi enter the urinary tract through an indwelling catheter. Around 15–25% of hospitalized patients receive a catheter, and nearly 75% of hospital-acquired UTIs are linked to them. CAUTIs not only cause patient discomfort but also extend hospital stays and increase healthcare costs, making them a key quality concern for hospitals.
Diagnosis and Clinical Presentation
Identifying catheter-associated urinary tract infections (CAUTIs) requires a two-step approach. The following are the key areas to assess: recognizing symptoms in patients with indwelling catheters and confirming findings through laboratory testing and defined diagnostic criteria.
Recognizing Symptoms in Patients with Indwelling Catheters
Signs often differ from classic urinary infection. Instead, look for fever, suprapubic tenderness, flank pain, or altered mental status—especially in older patients. Because catheters obscure normal voiding, vigilance is critical.
Laboratory Testing and Criteria for Diagnosis
Diagnosis requires both clinical symptoms and culture results. Surveillance data from NHSN show CAUTI rates in U.S. acute care hospitals ranging from 3.1 to 7.5 infections per 1,000 catheter-days. Some facilities show even wider ranges, up to 35.2 per 1,000 catheter-days depending on ward type.
Comparison of Asymptomatic Bacteriuria and Catheter-Associated UTI
In intensive care, one study observed CAUTI in 8.83% of patients (243/2,751) within 48 hours.
Prevention and Risk Reduction Strategies
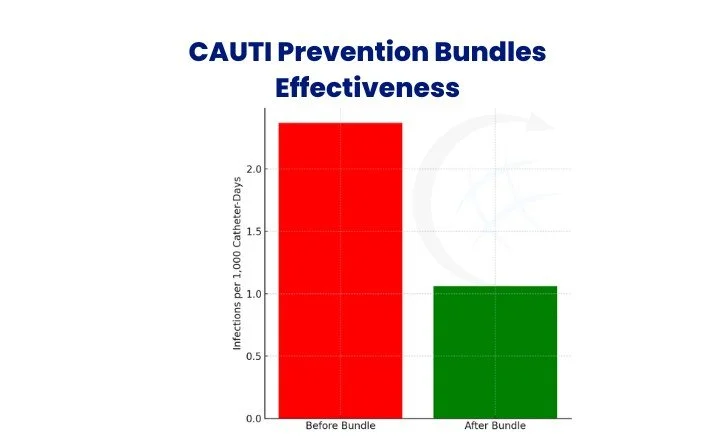
Preventing urinary catheter infections is feasible through proven interventions. Firstly, use aseptic technique during insertion. Secondly, remove catheters as soon as clinically possible. For example, VA’s Bladder Bundle yielded a drop from 2.37 to 1.06 CAUTIs per 1,000 catheter-days in medical units. Health Systems Research More broadly, CAUTI rates in non-ICU units fell by about 32% when bundled interventions were applied.
Use aseptic technique, daily review of catheter necessity, early removal protocols, and staff education to reduce risks.
Treatment and Management of Catheter-Associated
When treating catheter associated urinary tract infections, antibiotic therapy should be guided by urine culture results. At the same time, replacing or removing the catheter interrupts bacterial biofilm and helps antibiotics work effectively. On balance, treatment without catheter removal often leads to recurrence. In one center, implementation of maintenance protocols (including catheter practices) reduced CAUTI cases from 53 down to 9 in 4 years—an 83% drop.
ICD-10-CM Coding for Urinary Catheter Infections
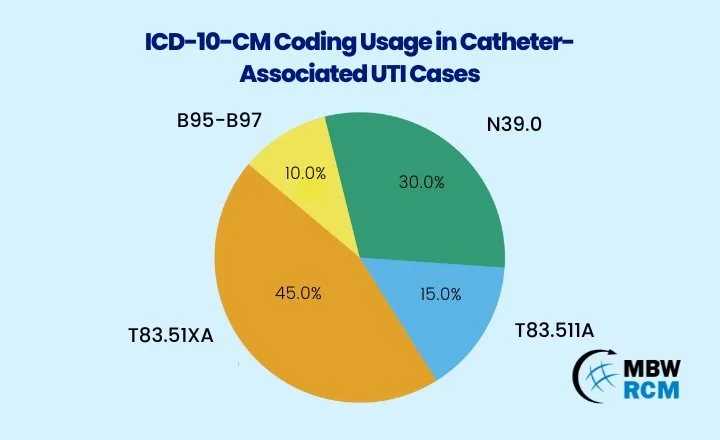
Correct coding of urinary catheter infections is important not only for reimbursement but also for compliance with hospital infection reporting programs. ICD-10-CM codes capture both the presence of the infection and, when applicable, the device causing it. This helps healthcare facilities track infection trends, meet federal quality metrics, and prevent reimbursement penalties.
Common ICD-10-CM Codes in UTI Cases
For more insight into coding practices, the guide on ICD-10 coding for catheter-associated infections offers coding scenarios, clarifies documentation requirements, and outlines common errors to prevent.
CPT Codes for Catheter Procedures
Billing depends on correct CPT selection for catheter insertion, replacement, or irrigation. Using the right code reduces denials and keeps claims compliant. A helpful overview of the most commonly used codes is available in this guide on CPT codes for urinary catheter insertions.
Coding Challenges and Documentation Pitfalls
Errors in CAUTI coding often arise when documentation and coding practices are incomplete or inconsistent. Below are some of the most common challenges and how they can be addressed.
Documentation omits explicit link between infection and catheter
Coders need clear documentation that specifies the UTI is caused by or associated with the catheter. Without this link, the diagnosis may default to a general UTI code (e.g., N39.0) instead of a catheter-related code, which impacts both reporting and reimbursement.
Colonization is mistaken for infection
Not every positive urine culture equals infection. Colonization may show bacteria without symptoms, while CAUTI requires both clinical signs and culture confirmation. Misclassifying colonization as infection leads to unnecessary coding, antibiotic use, and reporting errors.
Infecting organism codes (B95–B97) are omitted
Organism codes identify pathogens such as E. coli or Enterococcus, which are common in CAUTI cases. Leaving these codes out means the medical record lacks detail about the causative agent, making it harder for facilities to track infection trends and for payers to assess claims.
How Urology Clinics and Billing Services Handle CAUTI Cases
Correct CAUTI coding influences reimbursement outcomes and audit defense. Many practices rely on urology clinic billing services to manage evolving coding rules, ensure compliance, and reduce claim denials.
Future Trends in Diagnosis, Management, and Coding
The catheter infection treatment market is projected to grow from US$1,389.7 million in 2025 to US$1,960.4 million by 2035 (CAGR ~3.5%). Research is also advancing AI-enabled predictive modeling and new catheter designs aimed at preventing bacteria from entering the urinary tract. As coding and health tech evolve, mapping clinical algorithms to claim logic will receive increasing attention.
“Biofilm on catheters is bacteria’s version of building condominiums — once they settle in, it’s hard to get them out.”
In conclusion, managing catheter associated urinary tract infections requires vigilance in diagnosis, structured prevention, and effective treatment. Simultaneously, coding professionals must apply ICD-10-CM and CPT correctly to support reimbursement and compliance. With both clinical and administrative precision, CAUTI care improves patient outcomes and reporting accuracy.
For practices seeking support with CAUTI documentation, coding, or claims management, contact MBW RCM for guidance. Our team offers dedicated urology billing services to help reduce denials and keep your practice compliant.
FAQs: Catheter-Associated Urinary Tract Infections (CAUTI)
Request for Information
Are coding errors in catheter-associated urinary tract infection (CAUTI) claims slowing down reimbursements? Fill out the form below to learn how MBW RCM can support your practice with expert urology billing services.