Psychiatric E/M Codes vs. CPT Codes: What’s the Difference and How to Use Them
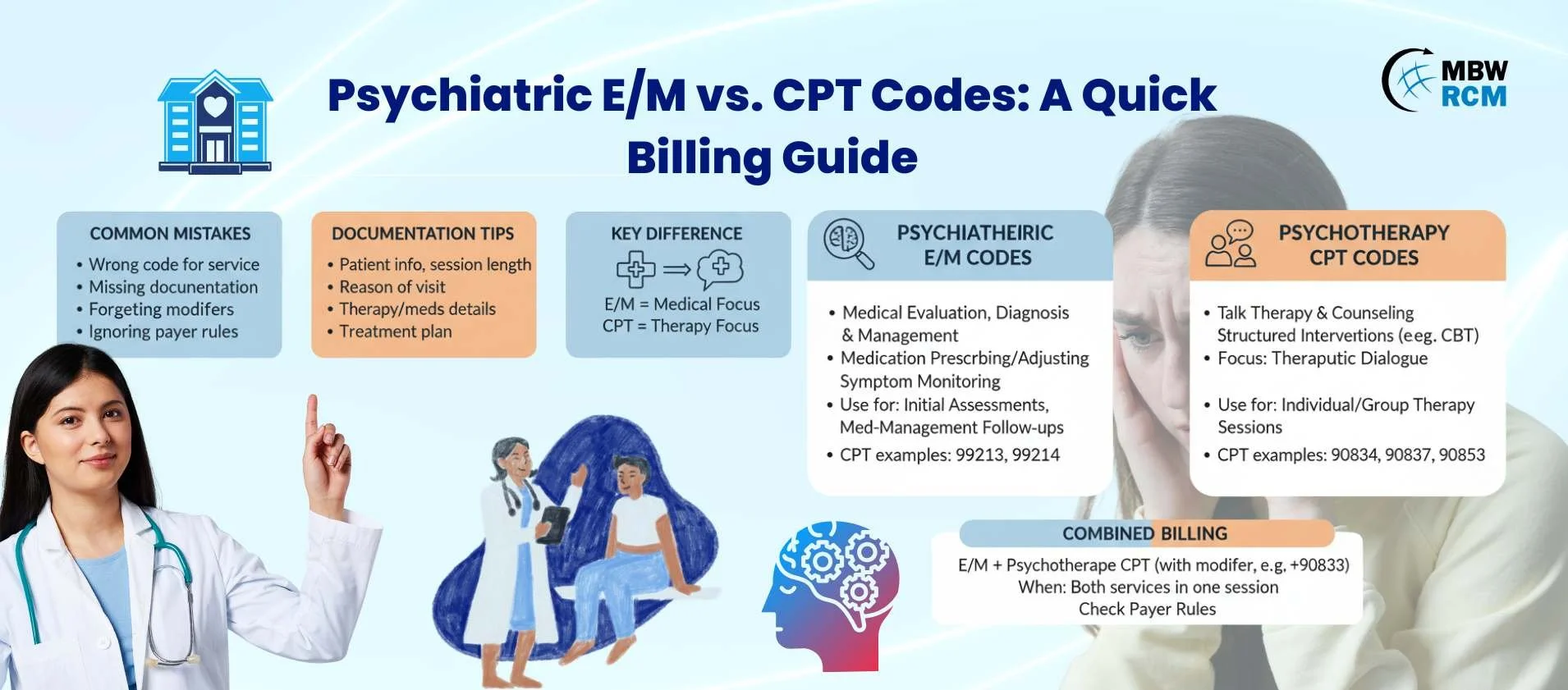
When billing for psychiatric services, many providers get confused about psychiatric E/M codes vs CPT codes. Both are used in mental health billing, yet they apply in different situations. Misunderstanding when to use them often leads to claim denials or lost revenue. This guide breaks down the differences and shows you how to apply them correctly.
Table of Contents
1. What Are Psychiatric E/M Codes?
Psychiatric E/M codes refer to Evaluation and Management services, such as CPT 99212–99215. These codes apply when psychiatrists provide medical assessments, prescribe medications, or manage treatment beyond psychotherapy.
Using E/M codes helps capture the complexity of psychiatric care, especially when both evaluation and medication management occur.
2. What Are CPT Codes in Psychiatry?
CPT codes in psychiatry include psychotherapy-specific services like 90832, 90834, 90837 (individual therapy) or 90853 (group therapy). These are used when providers deliver talk therapy, counseling, or structured psychotherapy without medical evaluation components.
Understanding the distinction between psychiatric E/M codes vs CPT codes prevents confusion during billing.
3. Key Differences Between E/M and CPT Codes
Although both apply to psychiatric services, they differ in use:
E/M codes → for medical evaluation, diagnosis, and management (e.g., prescribing).
CPT psychotherapy codes → for therapy sessions like CBT or group therapy.
Combined billing → sometimes both may be billed if therapy and medication management happen during the same visit.
“Think of E/M codes as the doctor’s toolkit and CPT codes as the therapist’s notebook.”
4. When to Use Psychiatric E/M Codes
Psychiatric E/M codes should be used when:
Conducting initial psychiatric evaluations.
Adjusting or prescribing medications.
Documenting symptom management or medical monitoring.
Always ensure documentation supports the level of service billed, such as CPT 99213 or 99214.
5. When to Use Psychiatric CPT Codes
CPT psychotherapy codes apply when:
Providing individual or group therapy.
Delivering counseling or structured interventions.
Sessions focus entirely on psychotherapy without medication adjustments.
For examples, review our guide on mental health billing codes.
6. Can You Bill Both E/M and CPT Codes Together?
Yes, in some cases. If a psychiatrist provides both psychotherapy and medication management in one session, you may bill an E/M code plus a psychotherapy CPT code with the correct modifier (e.g., +90833 for add-on psychotherapy).
Always check payer guidelines to confirm combined billing is allowed.
7. Common Mistakes in Using Psychiatric Codes
Frequent errors when choosing psychiatric E/M codes vs CPT codes include:
Using E/M codes without sufficient medical documentation.
Applying psychotherapy codes when medication management dominates.
Forgetting modifiers when billing both services.
Ignoring payer-specific rules.
Avoiding these mistakes improves claim acceptance rates. For additional insights on optimizing billing processes, check out our guide on outsourcing behavioral health billing.
8. Compliance and Documentation Tips
Proper documentation is critical. When billing psychiatric E/M codes vs CPT codes, always include:
Patient identifiers and session length.
Reason for the visit.
Details of therapy or evaluation performed.
Medication prescribed (if applicable).
Plan for treatment or follow-up.
For compliance resources, see the American Psychiatric Association’s billing tips.
FAQs: Psychiatric E/M Codes vs CPT Codes
Request for Information
Confused about psychiatric E/M codes vs CPT codes and when to use them? At MBW RCM, we help mental health providers bill correctly, reduce denials, and stay compliant. 👉 Request More Information by filling out the form below.