Reducing Patient Registration Errors: 8 Tips for Front-End Staff
Accurate patient registration is the first and most critical step in both healthcare revenue protection and patient safety. Every time a patient walks through your door, their journey — and your reimbursement process — begins with the information captured at the front desk.
When registration data is wrong, the fallout can be enormous: denied claims, delayed treatments, frustrated patients, strained provider-staff relationships, and millions of dollars in lost revenue.
The scale of the problem is bigger than most realize:
48% of healthcare leaders admit that their registration data is only “somewhat” or “not” accurate.
Even small typos can ripple through the system, causing errors in billing, misfiled patient records, or miscommunication between care teams.
In high-volume hospitals and practices, these tiny mistakes compound quickly — and they aren’t just administrative headaches; they can lead to clinical errors and loss of trust.
Table of Contents
The Industry’s Big Problem with Patient Registration
Front-end registration errors are not minor mishaps — they are systemic, costly, and preventable.
Key statistics paint the picture:
As data scientist Dean Abbott famously said:
“No data is clean, but most is useful.”
In healthcare, however, “useful” data isn’t good enough. It must be precise — every letter, every number, every field — because the cost of inaccuracy is simply too high.
Why Front-End Staff Are the Heroes of the Revenue Cycle
While physicians and billing teams often get the spotlight, the front-end staff are the gatekeepers to both the patient experience and the revenue cycle.
With most claim denials and compliance issues originating at registration, front-end staff have the power to:
Prevent revenue leakage before it starts.
Protect patient safety by ensuring records match the right person and coverage.
Build trust through transparent communication about financial responsibility.
Your work directly influences:
The likelihood of getting paid on time.
The patient’s trust in your organization.
The speed and quality of care they receive.
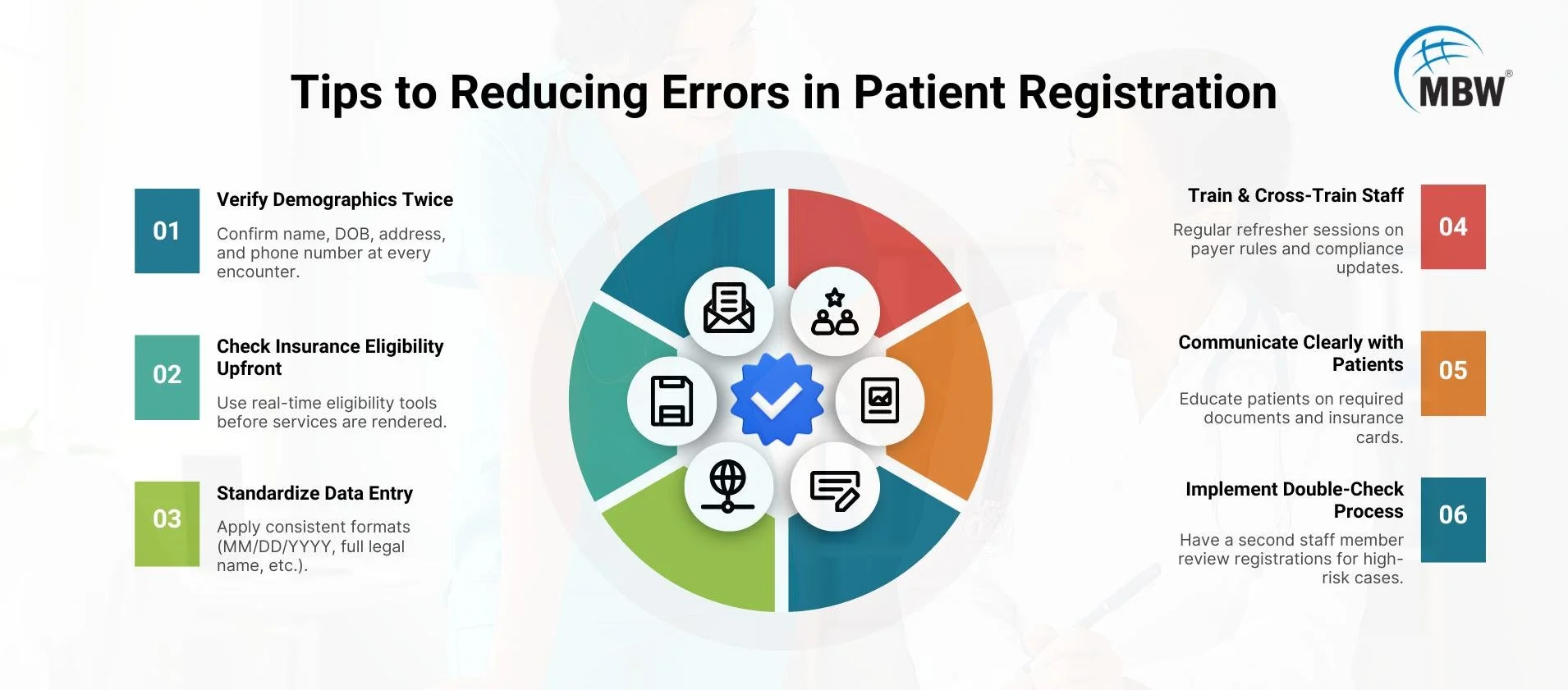
8 Proven Tips for Reducing Registration Errors
1. Thorough Identity Verification
Request two forms of ID every time (driver’s license, insurance card, passport, etc.).
Cross-check against existing records to prevent duplicates, which can cause billing errors, duplicate medical histories, and even patient safety risks.
2. Real-Time Insurance Verification
Confirm eligibility before any paperwork is completed.
Verify policy number, group number, coverage dates, plan type, and payer rules.
Don’t assume yesterday’s coverage is valid today — policies change more often than many realize.
3. Standardized Data Entry and Smart Forms
Use consistent formatting for names, addresses, and contact details (“Jonathan” vs. “Jon”).
Implement dropdown menus, autofill fields, and built-in validation to prevent typos and formatting errors.
Reduce free-text fields wherever possible — structured data is easier to validate.
4. Relentless Staff Training
Hold quarterly refresher courses on payer requirements, EHR updates, and process changes.
Share anonymized real-world denial cases to illustrate the financial and clinical consequences of mistakes.
5. Re-Verify at Every Visit
Even established patients should confirm their details at every encounter.
A simple “Have you moved?” or “Has your insurance changed?” can prevent a denied claim down the road.
6. Use Checklists and Surprise Audits
Develop a standardized intake checklist so no fields are overlooked.
Conduct random audits to keep accuracy high and highlight where retraining might be needed.
7. Radical Transparency on Payments
Clearly explain co-pays, deductibles, and outstanding balances upfront — before treatment begins.
Avoid situations like the infamous chart note:
“The patient left before payment could catch them.”
8. Leverage Technology for Error Prevention
Integrate your EHR and registration systems to enable real-time data validation.
Set up alerts for incomplete or illogical data entries (e.g., Medicare for a two-year-old).
Use automated insurance verification tools to instantly confirm coverage instantly, while focusing on the efficient patient onboarding in healthcare billing helps minimize denials and protect revenue.
Bonus Tip: The Buddy System
Before finalizing a registration, have a colleague review the details.
Four eyes are better than two — unless you’re all wearing the same glasses.
The Payoff: Why Accuracy Matters
When registration is done right, the benefits are both financial and relational:
Faster cash flow — clean registrations mean fewer claims kicked back for rework.
Lower denial rates — most denied claims never get resubmitted, so prevention is critical.
Better patient trust — no surprise bills, no mismatched records, no delays in care.
Given that hospitals lose $17.4 million annually in denied claims from registration errors, the ROI of accuracy is undeniable. Hospitals and practices that focus on accuracy can greatly improve outcomes, as shown in this case study on how we fixed patient registration delays.
Conclusion & Call to Action
Sloppy registration is not just an inconvenience — it’s a profit leak and a risk to patient care. With nearly half of healthcare data considered unreliable and millions lost every year due to preventable front-end errors, precision at intake is the keystone of a healthy revenue cycle.
At MBW RCM, our patient registration services help to
Deliver targeted training based on real-world case studies.
Implement technology integrations that flag and prevent costly errors.
Design workflow improvements that strengthen both revenue protection and patient satisfaction.
Because in healthcare, every patient matters — and so does every penny.
Contact MBW RCM today to turn your registration desk into a data-accuracy powerhouse that protects revenue and builds trust from the very first interaction.