Navigating the Coding Maze: How to Avoid the Most Common Coding Errors
Medical coding is a complex and highly specialized field that serves as the crucial link between clinical services and financial reimbursement. With thousands of codes, ever-changing guidelines, and strict payer rules, it's easy to make a wrong turn. Coding errors are a leading cause of claim denials, costing healthcare organizations billions each year in lost revenue and wasted time.
Think of a medical claim as a story told in a foreign language—the language of codes. If the translator (the coder) makes a mistake, the entire message is misunderstood, leading to a denial. This guide will help you navigate the coding maze by identifying the most common coding errors and providing actionable strategies to avoid them, focusing on ICD-10/ICD-11, CPT codes, modifiers, and bundling issues.
According to the Office of Inspector General (OIG), improper coding accounts for over $4 billion in Medicare overpayments each year. Avoiding these errors requires ongoing education, attention to detail, collaboration, and robust quality control.
“Accurate coding is not just about compliance—it’s about protecting the integrity of patient care and ensuring fair reimbursement.”
Table of Contents
1. ICD-10/ICD-11 Coding Errors
The Error: Using the wrong diagnosis code, failing to code to the highest specificity, or using outdated codes. Example: Coding “J45.909 – unspecified asthma” instead of “J45.20 – mild intermittent asthma” when documentation clearly supports the latter.
Impact: Leads to medical necessity denials, inaccurate data reporting, and potential compliance risks.
The Centers for Medicare & Medicaid Services (CMS) reports that insufficient specificity in ICD coding is a top-five cause of claim denials nationally.
How to Avoid It:
Specificity is Key: Always code to the highest level of detail supported by documentation.
Thorough Documentation Review: Check for additional details on severity, laterality, and etiology before finalizing codes.
Ongoing Education: Train staff regularly on ICD-10/ICD-11 updates and use reference tools.
Audit & Feedback Loop: Conduct quarterly audits and review error trends with coders.
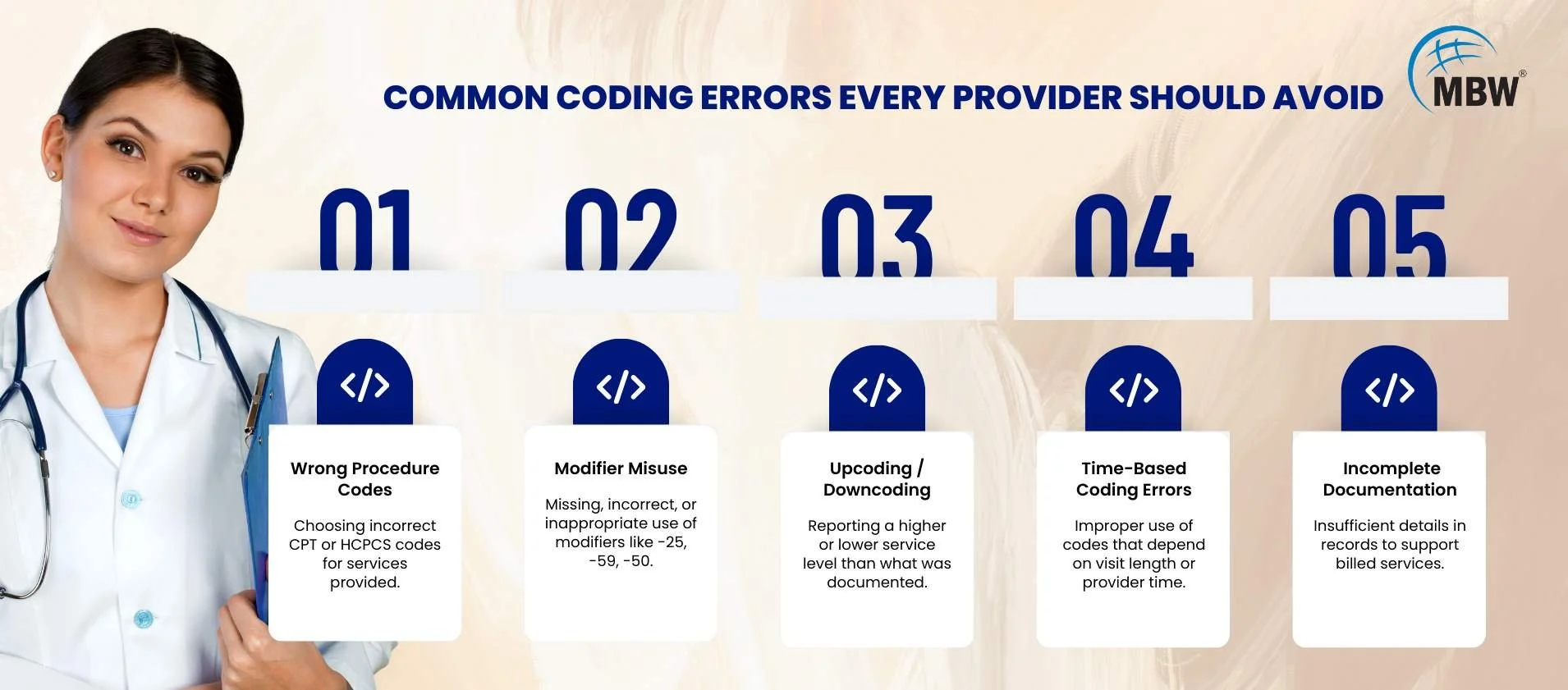
2. CPT Coding Errors
The Error: Selecting the wrong procedure code, misusing time-based codes, or omitting billable services. Example: Coding CPT 99213 instead of 99214 for a visit with documented moderate complexity can lead to underpayments and compliance risks. To reduce claim denials and improve coding accuracy, providers can reference this new patient CPT codes guide for proper documentation and code selection.
Impact: Lost reimbursement for undercoding, compliance risks for overcoding, and increased denial rates.
According to the AMA, CPT code misuse contributes to 12–15% of outpatient claim rejections.
How to Avoid It:
Procedure Note Review: Ensure the CPT code matches the service performed and documented.
Time-Based Code Accuracy: Document exact time spent when using time-dependent codes.
Annual CPT Training: Stay current with AMA updates and payer-specific coding rules.
Validation Tools: Use billing software with built-in CPT-to-diagnosis matching.
3. Modifier Misuse
The Error: Missing, incorrect, or inappropriate use of modifiers such as -25, -59, -50. Example: Omitting -59 for a distinct service performed on the same day, resulting in bundling and denial. A solid understanding of Commonly Used Modifier Codes in Medical Billing is essential to avoid these costly mistakes.
Impact: Increased claim rejections, compliance flags, and possible payer audits.
Industry Insight: The OIG has identified modifier misuse as a key compliance risk, noting that incorrect use of -59 alone leads to millions in improper payments annually.
How to Avoid It:
Know Payer Policies: Maintain an up-to-date modifier guide for top payers.
Training on NCCI Edits: Understand when modifiers override bundling rules legitimately.
Regular Audits: Monitor modifier use monthly to identify overuse or misuse patterns.
Documentation Alignment: Ensure modifiers are fully supported by chart notes.
4. Bundling and Unbundling Issues
The Error: Unbundling—billing separately for services that should be billed together—or over-bundling, missing legitimate separate services. Example: Billing incision and drainage separately when included in a larger procedure.
Impact: Denials, overpayment recoupments, and compliance investigations.
CMS data shows that bundling/unbundling errors account for roughly 10% of coding-related denials.
How to Avoid It:
Understand NCCI Guidelines: Familiarize coding teams with edits and payer-specific bundling rules.
Leverage Technology: Use claims scrubbing software to flag bundling errors before submission.
Case Reviews: For complex cases, have a second-level coding review to catch bundling errors.
5. Failure to Address Medical Necessity Denials
The Error: Perfect coding can still be denied if documentation doesn’t prove medical necessity. Often, coders fail to query providers for missing details.
Impact: Lost revenue from hard-to-overturn denials and increased rework.
Change Healthcare’s Denials Index notes that lack of medical necessity accounts for more than 40% of inpatient claim denials.
How to Avoid It:
Collaboration with CDI Specialists: Work together to ensure documentation fully supports codes.
Formal Query Process: Implement structured queries when notes are unclear, incomplete, or conflicting.
Provider Education: Train providers on documenting to payer medical necessity criteria.
The Path to Error-Free Coding
Achieving consistently accurate coding is not a one-time project; it’s an ongoing process that requires an organizational commitment to best practices, oversight, and adaptability. A truly error-free environment integrates quality assurance into every stage of the revenue cycle, from point-of-care documentation through final claim submission. This involves aligning coding policies with the latest regulatory changes, assigning clear accountability for error tracking, and maintaining an environment where coders can regularly refresh skills, ask questions, and collaborate with clinical and billing teams. Staying informed about common administrative mistakes in medical coding is also essential for preventing administrative concerns and supporting compliance.
Avoiding these mistakes requires:
Continuous Education: Ongoing updates on ICD, CPT, and modifier guidelines.
Cross-Functional Collaboration: Seamless communication between coders, providers, and billers.
Technology Investment: Automated compliance checks, predictive analytics, and denial prevention tools.
Regular Audits & Feedback: Use audit results to target coder training and process improvements.
“Clean claims don’t just happen—they are built on a foundation of accuracy, collaboration, and constant vigilance.”
MBW RCM Can Help
At MBW RCM, we guide healthcare organizations through the coding maze with expert audits, coder training, and compliance-driven processes. Our team stays current on ICD-10/ICD-11, CPT, modifier, and bundling rules, ensuring your claims are accurate, compliant, and paid faster.
📞 Contact us today to learn how we can help you eliminate coding errors, reduce denials, and optimize your revenue cycle.