New Patient Visit CPT Code: What’s New in 2025 Coding Updates
The New Patient Visit CPT Code is at the center of many billing changes in 2025. As a matter of fact, providers and coders must now consider updates that alter both evaluation and documentation. Accordingly, the 2025 coding updates bring modifications not only to descriptors but also to code applicability, particularly in telemedicine and AI-assisted visits.
Who Qualifies as a New Patient in 2025?
A "new patient" is defined as someone who has not received any professional services from a physician or qualified healthcare professional within the same group practice in the past three years. Without a doubt, understanding this distinction is the foundation for selecting the correct New Patient Visit CPT Code.
Updated CPT Code Range for New Patient Visits (99202–99205) in 2025
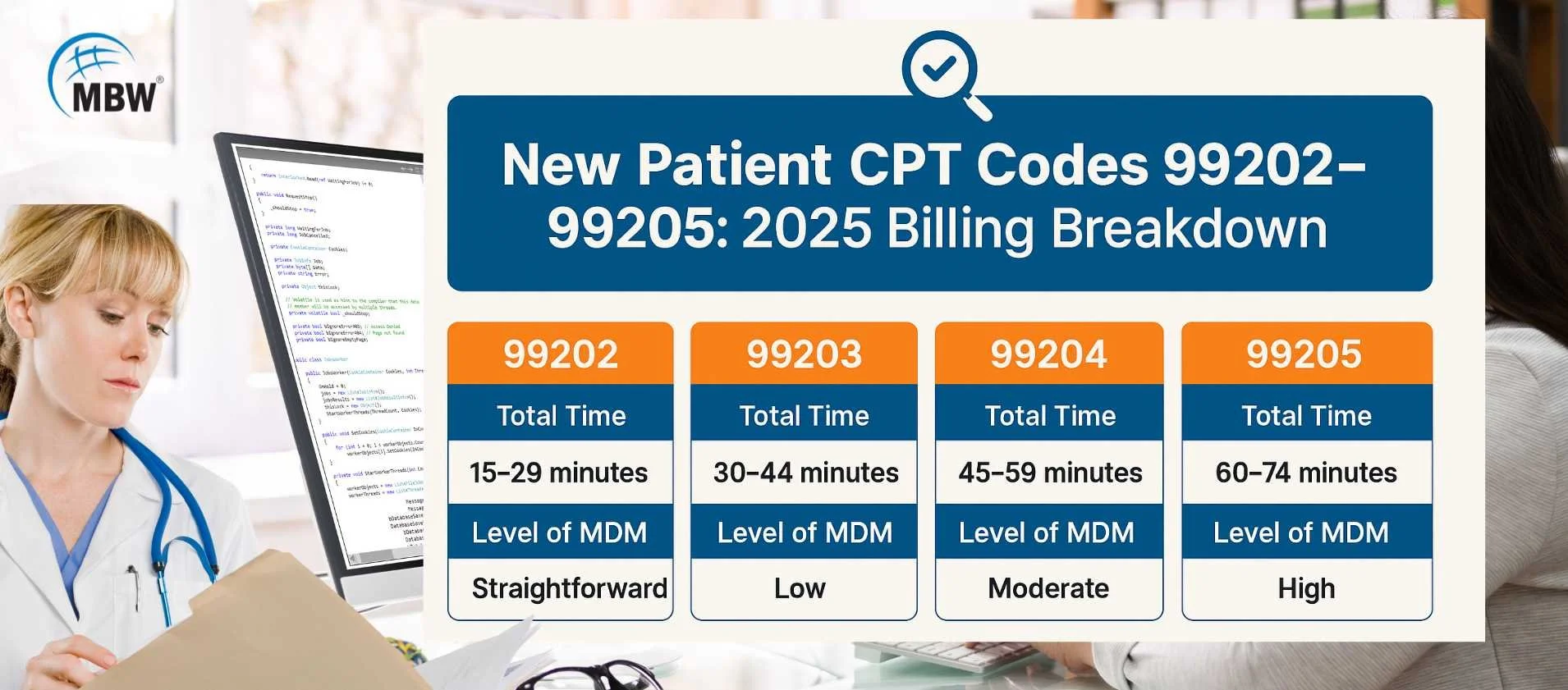
The New Patient Visit CPT Code range in 2025 includes CPT codes 99202 through 99205. Each code reflects the complexity and duration of the visit. Previously, CPT code 99201 was deleted and remains invalid in 2025. Not only does each code account for time, but it also reflects decision-making complexity. For a more detailed breakdown, visit our New Patient CPT Codes Guide.
Breaking Down Each New Patient Visit CPT Code
CPT Code 99202: When to Use It for Straightforward New Patient Visits
This code is used for visits involving straightforward medical decision-making and typically lasts 15–29 minutes. It is ideal for minor, self-limited conditions or routine checkups.
CPT Code 99203: Best for Low-Complexity New Patient Evaluations
This applies to visits requiring low-complexity MDM and usually ranges from 30–44 minutes. Common examples include stable chronic illnesses or multiple minor problems.
CPT Code 99204: Moderate-Complexity New Patient Visits
Designed for moderate-complexity cases, this code is used when the provider manages one or more chronic conditions or when diagnosis requires moderate effort. Time ranges from 45–59 minutes.
CPT Code 99205: Handling High-Complexity New Patient Encounters
This code is reserved for highly complex evaluations, including undiagnosed conditions with high risk or life-threatening issues. Time ranges from 60–74 minutes. For more detail, see our in-depth guide to New Patient CPT Codes.
Time-Based Coding: Duration Requirements for Each Code
In 2025, providers may choose time-based coding for New Patient Visit CPT Codes when medical decision-making doesn't determine the visit level. This includes total time spent on the encounter date, such as reviewing records, patient communication, and documentation.
| CPT Code | Time Range (Minutes) |
|---|---|
| 99202 | 15–29 |
| 99203 | 30–44 |
| 99204 | 45–59 |
| 99205 | 60–74 |
For visits lasting beyond 74 minutes, CPT code 99417 for prolonged services may be used with 99205. Be sure documentation supports the time billed and aligns with payer policies.
Required Documentation: History, Exam, and Medical Decision-Making
To correctly report a New Patient Visit CPT Code in 2025, the documentation must clearly support the complexity level or time being billed. Providers must document three key elements:
History: This includes relevant information about the patient’s current complaint, past medical history, family history, and social factors that may impact care. It should be tailored to the presenting problem and documented clearly.
Exam: The physical examination must be medically necessary and appropriate to the patient’s concerns. It may be limited to a specific system or cover multiple areas, depending on the condition.
Medical Decision-Making (MDM): MDM reflects the provider’s cognitive effort in assessing the patient. This includes the number and complexity of problems addressed, the amount and type of data reviewed, and the risk of complications or morbidity based on the treatment plan.
If billing by time, include total minutes spent and related tasks on the service date. When using AI tools, note their role in the documentation. Everything must support the selected CPT code and meet payer compliance standards. For a detailed reference on time-based coding and CPT code usage, visit the AAPC CPT Code Range.
How New Patient Codes Differ from Established Patient Visits
New and established patient codes differ in documentation and service level. New patient visits (99202–99205) require all three key elements: history, exam, and MDM or time. Established patient codes (99211–99215) may allow more flexible documentation based on the nature and complexity of the visit.
Here are the primary differences between the two types of codes:
| Feature | New Patient Codes (99202–99205) | Established Patient Codes (99211–99215) |
|---|---|---|
| Relationship Requirement | No professional service in past 3 yrs | Seen within past 3 years |
| Documentation Requirement | History, Exam, and MDM or Time | May require fewer components |
| Visit Complexity | Often higher, more detailed | Often focused, follow-up care |
| Code Selection | More detailed justification needed | Simpler for ongoing care |
Verify patient status using the 3-year rule to ensure correct code selection and reimbursement.
Telehealth, AI, and Modifier Rules in 2025
Telehealth remains integral to E/M coding in 2025, especially as virtual care becomes more common. New Patient Visit CPT Codes (99202–99205) are eligible for billing via telehealth if all documentation and platform requirements are met. Each service must be accurately identified using specific modifiers that inform payers about the nature of the visit or how it was documented. These modifiers help clarify if the service was delivered via telehealth, involved a separate procedure, or used AI-based documentation tools.
Here are the key modifiers commonly used when reporting new patient visits in telehealth or AI-supported settings:
| Modifier | Description |
|---|---|
| 95 | Indicates a real-time audio and video telehealth service |
| 25 | Signifies a separately identifiable E/M service on the same day as another procedure |
| AI | Identifies that documentation was supported or generated in part by AI tools |
Using the right modifier helps prevent billing errors and supports audits. Clearly indicate any AI-assisted documentation, and always follow payer-specific telehealth rules.
Billing Guidelines and Reimbursement Tips for New Patient Visits
To bill correctly using New Patient Visit CPT Codes, it's important to follow key steps that align with payer expectations and coding regulations:
Verify Patient Status: Use the 3-year rule to confirm the patient is truly new to the practice.
Choose Code Method: Decide whether to select the CPT code based on medical decision-making or total time spent on the visit date.
Apply Correct Modifiers: Use appropriate modifiers (e.g., 95 for telehealth, AI for AI-assisted documentation) to reflect service context.
Know Payer Policies: Check insurer-specific requirements for documentation, telehealth billing, and modifier use to avoid denials.
Staying up to date with payer guidance, coding updates, and documentation trends helps prevent rejections and supports timely reimbursement.
Top Mistakes When Using New Patient Visit CPT Codes
Avoiding common billing mistakes can prevent claim denials and compliance issues. Here are some of the most frequent errors coders and providers make when using New Patient Visit CPT Codes:
Misclassifying Patient Status: Billing a follow-up patient as "new" without applying the 3-year rule.
Unsupported Time-Based Coding: Selecting a code based on time without documenting all qualifying activities.
Omitting Required Modifiers: Failing to use necessary modifiers like 95 for telehealth or AI for AI-assisted notes.
Unvalidated AI Documentation: Relying on AI-generated records without clinician review or clear notation.
Being aware of these pitfalls helps maintain documentation integrity and supports faster, cleaner reimbursement.
Mastering New Patient Visit CPT Codes in 2025 means knowing how to apply time or MDM, document properly, and use the right modifiers. These updates impact your billing accuracy and audit readiness.
Need help applying these updates to your workflow? Explore MBW RCM for comprehensive revenue cycle management solutions, or contact our team for personalized support and expert CPT coding assistance.