Understanding CMS Place of Service Codes in Medical Claims
CMS Place of Service Codes identify where medical services are provided and are essential for accurate billing and reimbursement. Using the right POS code helps prevent denials, reduces delays, and ensures claims are processed correctly. This guide explains what POS codes are, where to report them, and how they impact billing in 2025.
What Are CMS Place of Service Codes in Medical Billing?
CMS Place of Service Codes refer to two-digit identifiers used to indicate where medical services were provided. These codes are reported on healthcare claims, especially CMS-1500 forms, to help payers understand the service location. Accordingly, each POS code corresponds to a specific care setting—such as an office, hospital, or patient’s home—used primarily for outpatient billing.
Why Are CMS Place of Service Codes Used in Healthcare Claims?
CMS Place of Service Codes are used to communicate the care environment where services occurred. Consequently, payers use these codes to determine reimbursement amounts, validate claim information, and ensure the billed CPT codes match the reported setting. If … then the wrong POS code is submitted, it can cause denials, reduced payments, or payer audits.
Where Are CMS POS Codes Used in the Claim Submission Process?
CMS Place of Service Codes are used during the medical billing process to show the setting in which the service was delivered. These codes are typically used for outpatient services, where the provider submits a bill for individual services performed (rather than for a full stay or procedure package). For a deeper understanding of how service codes influence billing accuracy and reimbursement, check out our guide on service codes for medical billing.
In the U.S., there are two main types of health insurance claim forms:
CMS-1500 – used by physicians, outpatient clinics, and other non-institutional providers
UB-04 – used by hospitals and institutional providers
Accordingly, CMS Place of Service Codes are mandatory on CMS-1500 forms. They help payers determine if the claim matches the procedure and the service location. Meanwhile, UB-04 forms do not use POS codes, but instead rely on revenue codes and Type of Bill indicators to describe services. Here’s how CMS Place of Service Codes are actually entered on the CMS-1500 form.
Reporting POS Codes on CMS-1500 Forms
The CMS-1500 form is the standard paper form used to bill Medicare Part B and many private insurers for outpatient services. This form has several fields where critical billing information is recorded.
One such field is Box 24B, which is specifically used to report the CMS Place of Service Codes. This two-digit code indicates where the patient was seen, such as an office (POS 11) or through telehealth at home (POS 10).
Example
If a patient visits their doctor at a clinic, the medical biller would enter POS 11 in Box 24B.
If the same visit happened via video call at the patient's home, POS 10 would be used instead.
POS Code Usage in UB-04 Claims: Is It Required?
The UB-04 form is used mostly by hospitals and inpatient facilities. These claims do not include a field for CMS Place of Service Codes. Instead, they use:
Revenue codes – to describe the department or service type
Type of Bill (TOB) – to classify the kind of institutional claim being submitted
Therefore, if you’re submitting an outpatient physician service, POS codes are essential. But if you’re billing for an inpatient hospital stay, POS codes are not part of the required data. Read more about billing and Place of Service codes.
List of CMS Place of Service Codes Used in 2025
CMS updates its POS code set regularly to reflect changes in care delivery. Using the correct CMS Place of Service Code is essential for getting claims approved and reimbursed on time.
CMS releases and updates its POS code set regularly. Below is a list of the most frequently used POS codes in 2025, along with clear definitions and typical billing use cases—covering office visits, telehealth, inpatient care, and more. so you know exactly which code to use, when, and why.
Most Frequently Used POS Codes in Medical Billing
| POS Code | Description | Typical Use Case |
|---|---|---|
| 11 | Office | Routine in-clinic appointments |
| 02 | Telehealth Provided Remotely (non-home) | Video visits from external locations |
| 10 | Telehealth Provided in Patient’s Home | Remote care where patient remains at home |
| 21 | Inpatient Hospital | Patients admitted overnight |
| 22 | On-Campus Outpatient Hospital | Clinic-based outpatient treatment |
| 23 | Emergency Room – Hospital | Hospital-based emergency services |
| 31 | Skilled Nursing Facility | Short-term rehab and skilled nursing services |
| 19 | Off-Campus Outpatient Hospital | Remote hospital departments |
| 49 | Independent Clinic | Standalone diagnostic or therapy clinics |
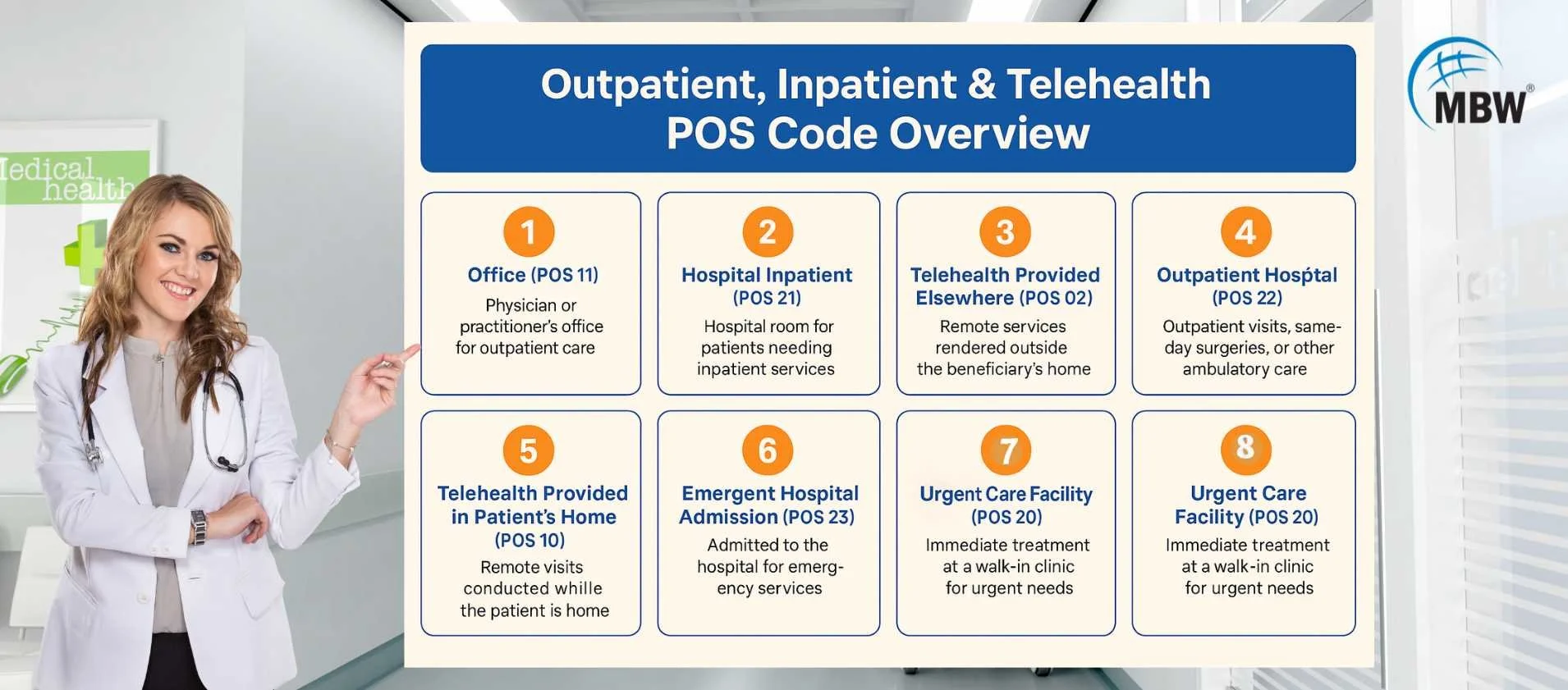
POS Code Chart for Outpatient, Inpatient, and Telehealth
This quick reference table groups CMS Place of Service Codes by care setting. Use it to easily identify which codes apply to outpatient visits, inpatient stays, and telehealth services—along with important billing notes for each.
| Setting Type | Common POS Codes | Billing Notes |
|---|---|---|
| Outpatient | 11, 22, 49 | Used for non-admitted services in various clinics |
| Inpatient | 21, 31 | Reserved for admitted or facility-based care |
| Telehealth | 02, 10 | Requires Modifier 95 in most payer policies |
Understanding Telehealth-Specific POS Codes: 02 vs 10
CMS introduced POS 10 to improve clarity in telehealth billing. Previously, POS 02 was used for all telehealth services. Now, POS 10 reflects care delivered while the patient is at home, whereas POS 02 applies to other remote settings.
Key Differences Between POS 02 and POS 10
| POS Code | When to Use It | What You Should Know |
|---|---|---|
| 02 | Use when the patient is not at home (e.g., clinic, school, mobile unit) | Still widely accepted; must add Modifier 95 to indicate real-time audio/video visit |
| 10 | Use when the patient is at home during the telehealth session | Specifically created for home-based care; also requires Modifier 95 for compliance |
Accordingly, POS 10 is now accepted by Medicare and many private payers, but billing teams must confirm payer policies beforehand.
When Should You Use POS 10 Instead of POS 02?
Use POS 10 when telehealth is delivered directly into a patient’s home—especially for routine follow-ups or mental health sessions. Use POS 02 for virtual visits in external clinics, schools, or other remote sites.
What Other Billing Elements Are Linked to CMS POS Codes?
Choosing the correct CMS Place of Service Code is only one part of clean claim submission. To avoid denials and delays, the POS code must align with other claim components like CPT codes, modifiers, provider addresses, and documentation. To avoid denials and get reimbursed correctly, your POS code must align with these five critical billing elements:
CPT Code Compatibility
Match the POS with the procedure code—wrong pairings can cause rejections or manual reviews.NPI and Provider Location
The POS must align with the billing location tied to your NPI to avoid mismatches.Modifiers (e.g., 95 for Telehealth)
Telehealth claims with POS 02 or 10 need Modifier 95 to confirm virtual service delivery.Visit Documentation
Your notes must support the POS code used—especially for telehealth or home services.Payer-Specific Edits
Some payers auto-deny claims when CPT and POS combinations don’t match their rules.
What Happens If You Enter the Wrong POS Code on a Claim?
Using the wrong CMS Place of Service Code can lead to payment issues, delays, and compliance risks. Below are five common problems that can occur: According to this CMS advisory on correct POS code usage, even small coding errors can cause claim denials or audits. Below are five common problems that can occur:
1. Claim Denials from POS Mismatch
Payers reject claims when the POS code doesn't align with the CPT code or service type. Example: billing an office visit (CPT 99213) with an inpatient POS (21) often gets denied.
2. Reduced Reimbursements
Incorrect POS codes can result in lower payments. POS 11 (office) typically pays more than POS 22 (outpatient hospital), even for the same service.
3. Delayed Processing
Mismatched POS codes may trigger manual reviews, especially for telehealth services without Modifier 95, delaying payments.
4. Risk of Payer Audits
Frequent POS errors increase the chance of post-payment audits or claim retractions, affecting provider trust scores.
5. Documentation Mismatch Triggers Audits
If the POS code on the claim doesn’t match the visit notes—like billing POS 11 (office) when the patient was actually at home—it can trigger payer reviews. Inconsistent records may lead to audits, payment takebacks, or provider flags.
Key CMS POS Code Changes You Should Know in 2025
CMS regularly updates Place of Service codes to reflect how care is delivered across settings—and 2025 brings some important changes. Understanding these updates is essential to avoid billing errors, missed reimbursements, or policy violations.
Here’s what’s changed in 2025:
| POS Code | What’s New | Why It Matters |
|---|---|---|
| 10 | Widely accepted by Medicare & private payers | Enables billing for home-based telehealth |
| 19 | Clarified definition for off-campus outpatient | Avoids confusion with POS 22 |
| 22 | Revised to better separate from POS 19 | Ensures proper hospital outpatient coding |
| 49 | Under tighter payer review | Risk of audit for clinic-based outpatient services |
| 11 | Increased scrutiny for certain outpatient claims | Prevents overuse in non-hospital billing scenarios |
To stay compliant and reduce claim rejections, providers should review CMS POS updates quarterly and check payer-specific implementation timelines.
How to Stay Compliant with CMS POS Code Requirements
Maintaining compliance with CMS POS codes means reducing errors, updating your systems, and training your team. Equally important, you need to keep documentation consistent with what you’re reporting.
Internal Audits, Quarterly Updates, and Staff Training
Review code usage through internal billing audits
Train billing staff on quarterly CMS updates
Verify EHR systems auto-fill POS codes correctly
Track denial trends to identify POS-related rejections
Outsourcing POS Review for Better Billing Outcomes
If POS management feels overwhelming, outsourcing it can help:
Expert teams verify code compatibility
Reduce claim denials and resubmission efforts
Improve payer communication and documentation readiness
Want clean claims and faster approvals?
Getting CMS Place of Service (POS) codes right can make all the difference in how quickly and correctly you get paid. At MBW RCM, we ensure that your POS codes align perfectly with the service, location, and documentation—so your claims move faster, with reduced rejections and far less stress.
Not sure if your team is using the right codes? Let us help you get it right the first time.
Talk to our billing experts today and make your claims cleaner and quicker to process.