NICU Coding and Billing Guide for Long-Stay Documentation
NICU coding and billing are critical components of managing neonatal intensive care, where newborns often require long hospital stays, specialized procedures, and complex documentation. Accordingly, understanding how to code for intensive and critical care procedures is essential for capturing the full scope of services provided to these vulnerable patients.
NICU Coding and Billing: Why It Matters for Long-Stay Newborns
NICU coding and billing deal with neonates who are not only premature but also medically fragile, often requiring weeks—or months—of intensive care. Both CPT and ICD-10 codes must reflect every intervention, diagnosis, and specialist interaction. After all, no sooner does one code lapse than billing errors and denials follow.
“NICU babies are like tiny time travelers—born too soon, yet carrying more documentation than a corporate merger.”
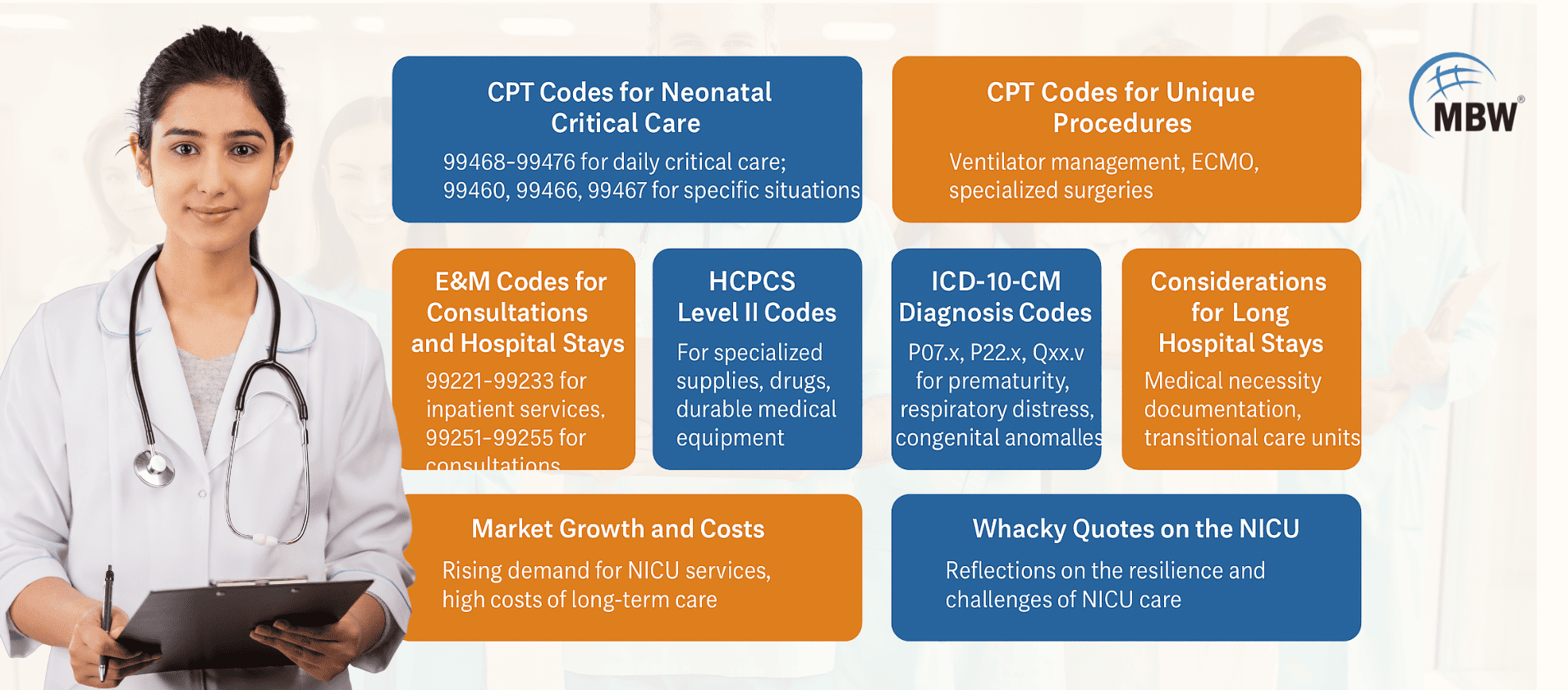
CPT Codes for Neonatal Intensive Care (NICU)
CPT codes for neonatal intensive care form the backbone of NICU billing. These codes are weight-based and categorized by the day of life:
99468–99469: Initial and subsequent critical care for infants <1500g.
99471–99472: For babies 1500–2500g.
99475–99476: For infants >2500g.
99460: Initial care for a neonate <30 days, not requiring critical care.
99466–99467: Transport of critically ill neonates.
As has been noted, assigning the correct weight-based code is essential, especially when coding changes mid-stay due to infant weight gain.
Coding Specialized Procedures in NICU
NICU patients often undergo highly specialized procedures, and CPT coding must reflect these accurately:
Ventilator Management (94002–94005): For both invasive and non-invasive respiratory support.
Central Line Access (36555–36573): For PICC lines or umbilical vein catheterization.
ECMO (33946–33947): Initiation and daily management codes for life support.
Exchange Transfusion (36450): Used in cases like hemolytic disease.
ROP Treatment (67031, 67028): For retinopathy of prematurity procedures.
“Coding a NICU chart is like trying to label every LEGO brick in a life-size spaceship—it’s technical, colorful, and someone will always step on a block you missed.”
ICD-10 Diagnosis Codes for Newborn Critical Care
NICU coding and billing requires precise ICD-10 coding to reflect the infant’s evolving condition:
P07.x: Disorders of prematurity and fetal growth.
P22.0: Respiratory distress syndrome.
P27.x: Chronic lung disease in neonates.
P59.x: Neonatal jaundice.
Q21.3: Congenital heart defect – Tetralogy of Fallot.
R68.82: Neonatal sepsis.
Comparatively, some conditions span both acute and chronic care, requiring updated ICDs over time.
Handling Prolonged NICU Stays: Billing and Documentation
Long-stay newborns may accumulate hundreds of billable interactions. Therefore:
Use time-based CPTs when appropriate (e.g., prolonged physician services).
Document daily status and rationale for critical care.
Clearly denote transfers between NICU, NTCU, and general pediatrics.
Avoid bundled-service errors for ventilator management or central access.
For insights on how healthcare providers can recover revenue from denied claims, especially in prolonged NICU cases, explore this guide on neonatal billing and NICU claim recovery.
💻 “A NICU progress note isn’t a ‘note’—it’s the neonatal version of War and Peace, except with more abbreviations and less romance.”
U.S. NICU Billing Trends and Industry Challenges
NICU billing in the United States presents a unique mix of high acuity care, payer-specific rules, and intensive documentation demands:
High NICU Costs: The average NICU stay in the U.S. exceeds $76,000, with some extreme cases reaching $500,000.
Medicaid and Private Insurance Variance: Coding and reimbursement rules can vary widely by payer.
DRG Models and Documentation: Bundled payment models require exact documentation for justification.
Shortage of Neonatal Coders: This leads to higher denial rates and claim delays in some facilities.
To understand how NICU systems and costs are evolving in the U.S., explore March of Dimes’ NICU guide, which provides a detailed nonprofit perspective on NICU care levels and family experiences.
Common Coding Pitfalls and Transition Errors in NICU Cases
Missing Medical Necessity Notes
Incorrect Transition Coding
Bundling Misunderstandings
Post-Surgical Global Period Errors
In like manner, always review payer contracts to know what's bundled and what qualifies as separately billable.
Top Procedures Performed in NICUs (and How to Code Them)
NEC Surgery (44180): Laparotomy for necrotizing enterocolitis.
PDA Ligation (33619): Surgical closure of patent ductus arteriosus.
ROP Laser Therapy (67031): For advanced retinopathy.
Dialysis Access (36556): For neonates requiring renal support.
Myelomeningocele Repair (63700): Complex neurosurgery in early life.
For more on neonatal surgical outcomes and NICU interventions, refer to Children’s Hospital Association’s surgical quality insights.
Documentation Tips for NICU Billing Accuracy
Be specific with birth weight, gestational age, and device use.
Include start and end times for time-based codes.
Use clear justifications for continued critical care.
Track team communications and parental counseling.
At this point, even automation tools can’t replace a detailed, coder-friendly narrative.
Best Practices for NICU Coders and RCM Teams
Stay up-to-date on CPT/ICD code changes.
Train coders in neonatal care terminology.
Conduct monthly documentation audits.
Use neonatal-specific EHR logic.
To streamline workflows, consider partnering with experts who provide NICU billing and coding services tailored to neonatal providers.
🤹 “NICU coding is like juggling flaming torches… while the baby’s chart grows five new arms.”
FAQs about NICU Coding and Billing
1. What are the main CPT codes used in NICU billing?
Codes 99468–99476 are used depending on weight and day of care. Codes for ventilator support, transport, and ECMO may also apply.
2. How is neonatal intensive care documented for insurance?
Accurate coding depends on clear documentation of diagnosis, interventions, provider time, and transition of care levels.
3. What diagnosis codes are common in NICU settings?
Frequent ICD-10 codes include P07.x for prematurity, P22.0 for RDS, and R68.82 for sepsis. Q codes are common for congenital anomalies.
4. How do U.S. hospitals manage prolonged NICU stays?
Hospitals depend on EHR tracking, payer-specific coding compliance, and detailed justification for each day of intensive care.
5. What are common NICU coding errors to avoid?
Top mistakes include unbundled procedures, missed global periods, and insufficient documentation for medical necessity.