Allergy & Immunology Billing Essentials: CPT, ICD-10 and Modifiers Every Practice Must Know
If you run an Allergy & Immunology practice, you already know how challenging billing can be. Between specialized allergy testing codes, immunotherapy injections, and payer-specific rules, even small mistakes can lead to denials, compliance risks, or lost revenue.
The good news? By mastering CPT codes, ICD-10 mapping, and correct modifier usage, you can avoid many of the common billing headaches and keep your revenue cycle flowing smoothly.
Here’s MBW RCM’s insider guide to making Allergy & Immunology billing work for you.
Table of Contents
Why Allergy Billing Is Tricky (and Why It Matters)
Allergy and Immunology services often combine office visits, diagnostic testing, and therapeutic procedures within the same patient encounter. This creates added complexity for coding and billing teams because they must:
Accurately assign multiple CPT codes per encounter to reflect all services delivered (e.g., an evaluation, skin testing, and immunotherapy injections in a single visit).
Provide precise ICD-10 documentation that establishes clear medical necessity for each service, linking the diagnosis to the procedure.
Apply the correct modifiers to signal to payers when services are distinct and should not be bundled together for payment purposes.
If your billing team doesn’t address these nuances with care, your practice may face avoidable claim rejections, delayed reimbursements, or compliance risks, all of which directly impact revenue cycle performance. To better understand how outsourcing can simplify this process, read how outsourcing transforms the Allergy and Immunology revenue cycle.
Step 1: Master CPT & ICD-10 Codes
Choosing the right codes isn’t just about memorizing lists — it’s about understanding how payers interpret them. Each CPT or ICD-10 code carries reimbursement and compliance implications, so practices need to connect the dots between patient presentation, documentation, and billing.
Common ICD-10 Codes
These diagnosis codes are frequently used in Allergy & Immunology, and they help demonstrate medical necessity:
J30.1 – Allergic rhinitis due to pollen (a common seasonal allergy scenario)
J45.909 – Unspecified asthma, uncomplicated (often used for general asthma when details are limited)
T78.1XXA – Other adverse food reactions (first encounter for food-induced allergic reactions)
D80.1 – Nonfamilial hypogammaglobulinemia (immune deficiency requiring ongoing monitoring)
Essential CPT Codes
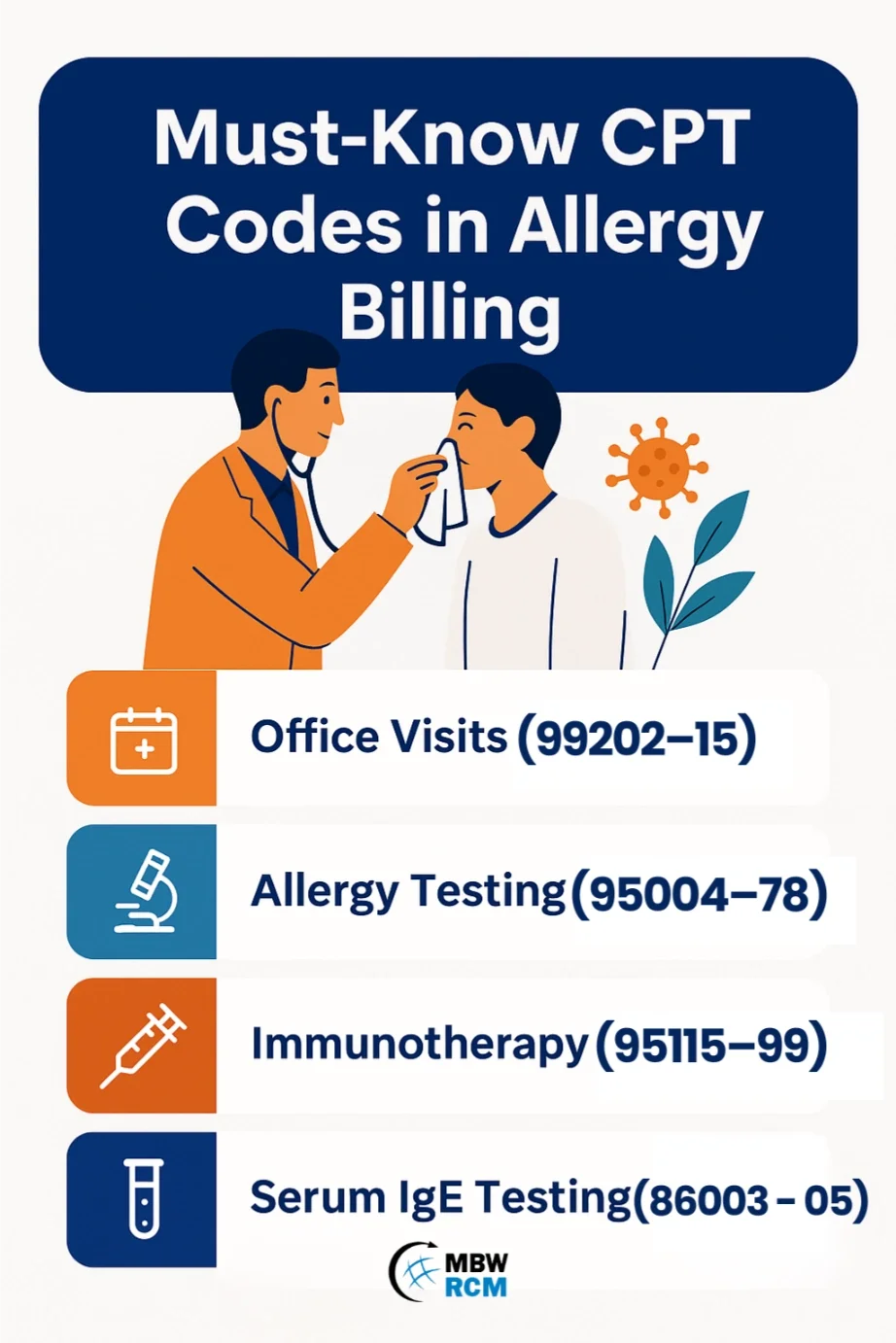
CPT codes describe the services performed. In Allergy billing, these codes often overlap in the same visit:
Office Visits (99202–99215) – Routine evaluation & management, which may include assessing allergy history or asthma management.
Allergy Testing (95004–95078) – Covers a range of diagnostic testing such as skin prick, intradermal, and patch testing. Documentation must specify number and type of allergens.
Immunotherapy (95115–95199) – Includes both the preparation of allergen extracts and the administration of allergy shots. Correct sequencing is key to reimbursement.
Serum IgE Testing (86003, 86005) – Blood-based allergy testing, particularly useful when skin testing isn’t appropriate (e.g., severe dermatitis or medication interference).
For example, billing 95004 (skin testing) with J30.1 (allergic rhinitis due to pollen) helps ensure payer approval.
Step 2: Decode Allergy Testing Codes
Allergy testing is one of the most commonly billed—and frequently denied—services, in part because of how payers view medical necessity and documentation. To ensure success, practices must clearly justify why each test was ordered, how it was performed, and what the clinical rationale was.
95004 – Skin Prick Testing: Bill per allergen tested. Each allergen must be listed in the record, and the provider should note the patient’s history (e.g., suspected pollen allergy) to justify the volume of tests.
95024 – Intradermal Testing: Used to confirm or expand on prick test results when suspicion remains high but prick testing is inconclusive. Documentation should explain why intradermal testing was necessary in addition to skin prick.
95044 – Patch Testing: Billed per patch, typically used to evaluate delayed hypersensitivity reactions such as contact dermatitis. Records must specify the allergens applied and the timing of readings.
86003 – Serum IgE Testing: A blood-based test for allergen-specific antibodies. Often ordered when skin testing is contraindicated (e.g., severe eczema, patient on antihistamines). Ensure that the documentation highlights why serum testing was chosen over skin testing. For detailed guidance on coding requirements, refer to this article on allergy testing and immunotherapy coverage.
Step 3: Use Modifiers the Right Way
Modifiers are your secret weapon to prevent denials—if used correctly. In Allergy & Immunology billing, they communicate the context of services and prevent payers from mistakenly bundling or denying legitimate charges.
Modifier 25 – Use when a significant, separately identifiable E/M service is performed on the same day as a procedure. This often applies when you see a patient for a new or established visit and also provide allergy testing.
Example: A new patient evaluation (99204) plus skin testing (95004) where the E/M service addressed history, exam, and management decisions beyond the testing itself. Documentation should clearly separate the two services.Modifier 59 – Use for distinct procedural services that might otherwise be bundled. For Allergy practices, this can occur when multiple types of tests (e.g., prick and intradermal) are billed in one encounter.
Example: Different allergy tests performed in the same visit, justified by separate clinical indications. Always note the reason each test was necessary.Other Modifiers:
76 – Repeat procedure by the same provider, such as repeating a test within the same day due to inconclusive initial results.
95 – Telehealth services, applied when patient consultations or follow-ups are conducted via telemedicine platforms.
For example, if you append Modifier 25, auditors expect to see evidence that the E/M service was medically necessary and distinct from the procedure performed.
Step 4: Denial-Proof Your Claims
The most successful practices follow a billing playbook to avoid common pitfalls and proactively address payer concerns. Allergy claims are especially vulnerable to denials due to reasons such as exceeding payer limits on the number of allergens tested, missing prior authorizations for immunotherapy, or insufficient documentation linking symptoms to test results.
Link ICD-10 to CPT codes properly to show medical necessity. For example, connect seasonal rhinitis diagnoses with specific pollen testing codes.
Be detailed in documentation—list each allergen tested, the patient’s symptoms, and the rationale for testing. Insufficient notes are a common denial reason.
Apply modifiers carefully and only when supported by the record. Payers often flag Modifier 25 or 59 if justification is weak.
Train your staff on allergy-specific billing requirements, such as payer rules on maximum number of tests per visit.
Audit your claims regularly to catch errors before payers do, and track denial trends to identify recurring issues that need process improvement.
Conclusion: The RCM Advantage
In Allergy & Immunology, every code, modifier, and diagnosis matters. Billing mistakes aren’t just inconvenient—they can directly impact your bottom line.
That’s why many practices turn to MBW RCM for expert support. Our team specializes in Allergy & Immunology billing, helping practices:
Reduce denials
Capture all eligible revenue
Stay compliant with payer and regulatory rules
Because at the end of the day, your focus should be on patient care, not billing errors.
Ready to tighten up your allergy billing?
Book a free mini-audit with MBW RCM to identify coding gaps and quick wins in your revenue cycle. Contact us today.