Top 5 Payer Challenges in ABA Billing and How to Overcome Them
For ABA practices, getting reimbursed is rarely as simple as submitting a clean claim. Insurance payers have complex rules, strict documentation standards, and long review cycles. Studies show ABA billing denial rates can reach 20–30%, much higher than other outpatient services.
In this blog, we break down the top five payer challenges in ABA billing—and share strategies to help your practice overcome them.
Table of Contents
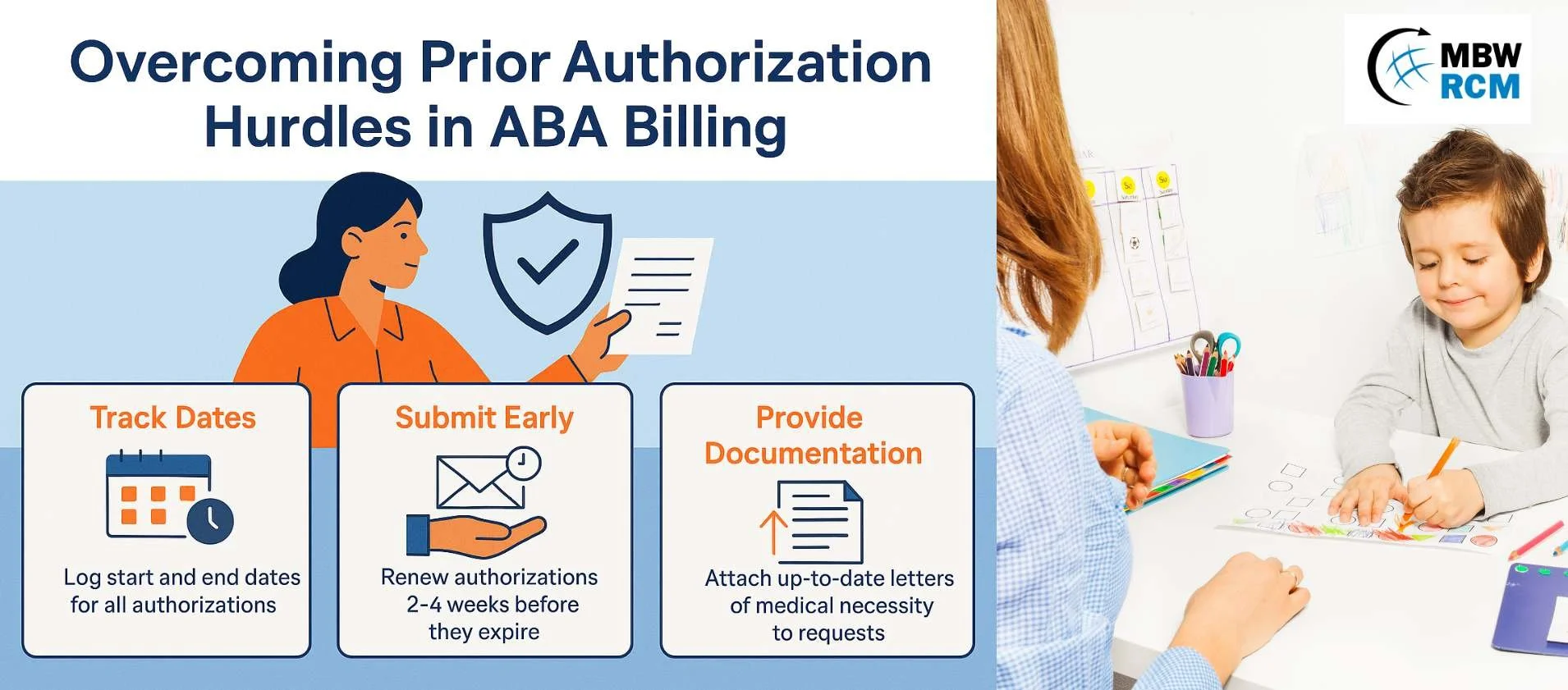
1. Prior Authorization Hurdles in ABA Billing
The challenge: Because ABA therapy often involves 20–40 hours of care per week, insurers rely heavily on prior authorizations (PA) to control costs. Denials happen when authorizations expire, exceed approved hours, or don’t include proper documentation.
How to overcome it:
Track PA start and end dates with reminders.
Submit renewals 2–4 weeks early.
Attach updated letters of medical necessity with every request.
Our ABA billing services include full PA management to help providers avoid costly treatment gaps.
2. Documentation Gaps and Medical Necessity
The challenge: Payers require detailed session notes, signed treatment plans, and progress reports to prove services are medically necessary. Missing details—like time stamps, goals, or parent signatures—are a leading cause of denials.
How to overcome it:
Use standardized documentation templates across the team.
Audit session notes weekly to ensure they match billed codes.
Update treatment plans every 6 months to reflect client progress.
The Substance Abuse and Mental Health Services Administration (SAMHSA) emphasizes that consistent documentation is a cornerstone of payer compliance across behavioral health services.
3. CPT Code Confusion in ABA Claims
The challenge: ABA services use unique CPT codes (97153, 97155, 97156, 97158). Errors—like billing the wrong code or missing modifiers—often lead to denials or audits.
How to overcome it:
Train billing staff on ABA-specific codes and modifiers.
Ensure session notes clearly support the code billed.
Use software that flags coding inconsistencies.
In one ABA billing case study, correcting code usage reduced denials by nearly 25% in just three months.
4. Payer Policy Variability Across States and Plans
The challenge: Every payer—and sometimes every plan—has different rules for ABA. Some restrict parent training, others cap supervision hours. Keeping track of these nuances is time-consuming but necessary.
How to overcome it:
Build a payer policy library for reference.
Assign a compliance lead to monitor changes.
Always verify benefits before beginning services.
The National Association of Insurance Commissioners (NAIC) advises providers to review state-specific payer regulations regularly, since coverage rules often shift. For additional guidance, see the NCSL’s summary of state autism insurance laws.
5. Delayed or Denied Reimbursements
The challenge: Even when claims are correct, payers often slow down reimbursements by requesting additional info or delaying high-dollar claims. For small ABA practices, delayed cash flow can be a major challenge.
How to overcome it:
Submit claims within 24–48 hours of service.
Monitor aging reports weekly.
Escalate delayed claims with appeals or payer follow-ups.
Our insights on ABA therapy and insurance processes show that consistent follow-up is the single biggest factor in reducing reimbursement cycles.
Turning Payer Challenges Into ABA Billing Solutions
Payer challenges are a reality in ABA billing—but they don’t have to overwhelm your practice. By strengthening authorization tracking, tightening documentation, coding correctly, and monitoring payer rules, ABA providers can reduce denials and improve cash flow.
Partnering with specialists like MBW RCM allows practices to focus on care while experts handle payer-specific complexities.
Frequently Asked Questions on ABA Billing Payers
Request for Information
Struggling with payer challenges in ABA billing? At MBW RCM, we help providers handle prior authorizations, improve documentation, and resolve denials quickly.