The Documentation Audit: Your A–Z Checklist for Bulletproof ABA Claims
In ABA therapy, documentation is the backbone of both quality care and successful billing. It proves medical necessity, tracks progress, and satisfies payer requirements. But when documentation is missing or inconsistent, insurers often deny claims—even for services you’ve already delivered.
The Office of Inspector General (OIG) found that nearly 42% of ABA therapy claims audited had documentation issues, ranging from missing progress notes to incomplete treatment plans. That’s why a thorough documentation audit is critical for ABA providers.
This guide provides an A–Z checklist to help you create bulletproof documentation and keep your ABA claims audit-ready at all times.
Table of Contents
Why Documentation Is Non-Negotiable in ABA Billing
ABA services are long-term, intensive, and highly individualized. Insurers scrutinize claims because therapy hours often run 20–40 per week for children with autism. Documentation must:
Demonstrate medical necessity through diagnostic and treatment evidence.
Match the details in prior authorizations.
Show measurable progress toward goals.
Without these, claims risk denials or even post-payment recoupments. As one BCBA put it: “In ABA, if it isn’t documented, it didn’t happen.”
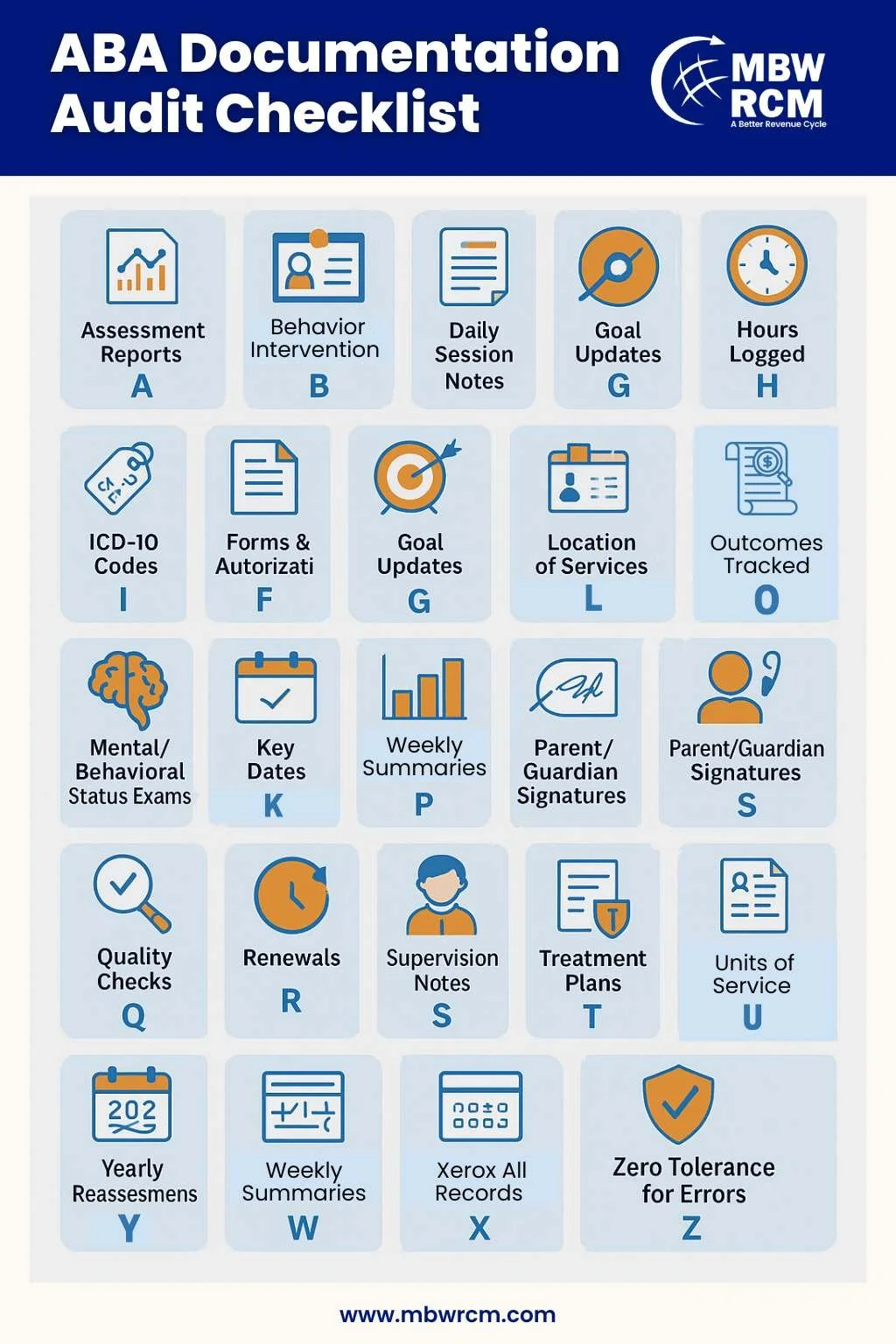
The A–Z Documentation Audit Checklist
Here’s your complete guide for reviewing ABA documentation before claims submission.
A – Assessment Reports
Include comprehensive initial and ongoing assessments that justify therapy.
B – Behavior Intervention Plans (BIPs)
Goals must be individualized, measurable, and based on baseline data.
C – Credentials of Providers
Keep licenses, NPIs, and certifications updated.
D – Daily Session Notes
Log start/end times, techniques used, and client response.
E – Evaluation of Progress
Progress notes should show measurable changes tied to goals.
F – Forms and Authorizations
Use correct payer forms; verify active prior authorization.
G – Goal Updates
Revise goals at least every 6 months—or sooner as needed.
H – Hours Logged
Make sure documented hours match billed hours.
I – ICD-10 Codes
Link claims and plans to valid diagnostic codes.
J – Justification Letters
Add letters of medical necessity for renewals or higher service hours.
K – Key Dates
Track plan start dates, authorizations, and expirations.
L – Location of Services
Specify setting (home, school, clinic) with correct service codes.
M – Mental/Behavioral Status Exams
Provide baseline and updated evaluations.
N – Notes Consistency
Align daily notes with treatment goals.
O – Outcomes Tracked
Use quantifiable data (e.g., “initiated peer interaction 4 times”).
P – Parent/Guardian Signatures
Required for in-home sessions in many payer contracts.
Q – Quality Checks
Audit internally at least monthly.
R – Renewals
Request authorization renewals well in advance.
S – Supervision Notes
BCBA supervision of RBT sessions must be logged.
T – Treatment Plans
Include frequency, duration, goals, and expected outcomes.
U – Units of Service
Check that billed units match session time and payer rules.
V – Verification of Attendance
Maintain signed attendance logs.
W – Weekly Summaries
Summarize progress beyond daily notes.
X – Cross-Check Claims
Match CPT codes, dates, and documentation.
Y – Yearly Reassessments
Conduct annual re-evaluations with updated goals.
Z – Zero Tolerance for Errors
Set a strict policy for complete, compliant documentation.
Common Mistakes That Trigger ABA Claim Denials
Copy-paste session notes (“cloned” documentation).
Missing time-in/time-out stamps.
Expired authorization dates tied to billed claims.
Stale goals that don’t reflect client progress.
These may seem small but can cause costly denials or audit penalties.
If you are interested to read more about ABA Therapy, please have a look at this blog on ‘‘ABA Therapy for Autism: What It Is, How It Works, and Who Benefits’’.
Staying Audit-Ready All Year
Standardize Templates: Use consistent formats for notes and treatment plans.
Train Staff Regularly: Keep BCBAs and RBTs aligned with payer requirements.
Leverage Billing Software: Technology can flag missing data or expired authorizations.
Consider Outsourcing: Specialists can manage documentation audits and reduce denial rates.
Our ABA therapy billing services support providers with audits, authorizations, and claims. See how one practice improved compliance in our ABA billing case study.
Industry Trends in Documentation
Audit frequency is rising: Insurers are reviewing ABA claims more closely.
Digital records are the new norm: Cloud-based EHRs help providers centralize notes.
Compliance risks are higher: Missing documentation can lead to repayment demands.
The Centers for Medicare & Medicaid Services (CMS) outlines documentation standards used during payer audits, while the National Institute of Mental Health (NIMH) highlights why autism treatment is closely monitored.
FAQs: ABA Billing Documentation Audits
Request for Information
Worried about documentation errors causing denials? At MBW RCM, we help ABA providers audit documentation, build compliance, and protect revenue.